Introduction
Acute injuries such as sprains, strains, and soft tissue trauma are common in sports, workplaces, and daily activities. Rapid pain relief and inflammation control are essential to prevent further tissue damage and to accelerate recovery. Traditional first aid methods, such as ice packs, compression, and elevation, are effective to some extent but often provide limited precision and speed. CO₂ Cryotherapy, a form of localized cold therapy using carbon dioxide gas, has emerged as a non-invasive, rapid, and highly targeted alternative. By leveraging vasoconstriction, reduced inflammatory mediator activity, and enhanced microcirculation, CO₂ Cryotherapy offers immediate symptom relief. This article explores its mechanisms, clinical applications, safety considerations, and integration with conventional first aid for acute injury management.
1. What Is CO₂ Cryotherapy?
Before exploring its first aid applications, it is essential to understand what CO₂ Cryotherapy is and how it differs from other cold therapy methods.
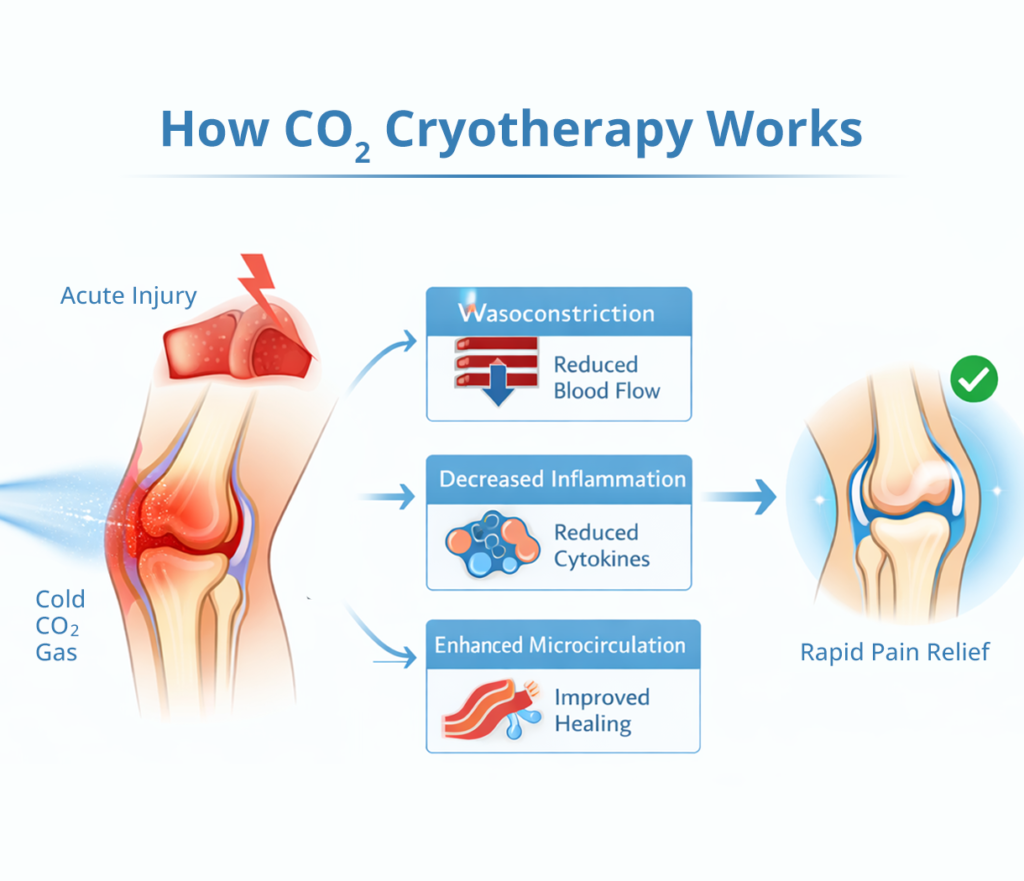
1.1 Mechanism of Action
CO₂ Cryotherapy works by rapidly cooling localized tissue using pressurized carbon dioxide gas at temperatures typically between -78°C to -80°C. This targeted cooling induces vasoconstriction, limiting excessive blood flow and reducing edema formation. Additionally, CO₂ Cryotherapy influences inflammatory mediators such as cytokines and prostaglandins, decreasing their release and limiting the inflammatory cascade. At the cellular level, cold exposure can modulate nociceptor activity and inhibit nerve conduction velocity, which directly reduces acute pain sensations. Moreover, reactive hyperemia occurs after short treatment cycles, promoting oxygenation, nutrient delivery, and collagen synthesis. This combination of vascular, cellular, and biochemical effects makes CO₂ Cryotherapy particularly suitable for immediate intervention in acute injuries.
1.2 Difference from Other Cryotherapies
Unlike traditional ice packs or cold-water immersion, CO₂ Cryotherapy provides highly controlled, precise, and dry cooling. Traditional methods often result in uneven tissue cooling, prolonged application times, and patient discomfort. Liquid nitrogen cryotherapy, on the other hand, is extremely cold and can damage healthy tissue if not carefully applied. CO₂ Cryotherapy occupies a therapeutic middle ground: it is cold enough to induce effective analgesia and reduce inflammation but safe enough to be applied quickly without extensive preparation. Furthermore, it allows clinicians to target specific joints, tendons, or muscle groups with minimal collateral tissue exposure, making it ideal for first aid scenarios in sports and occupational settings.
2. Acute Pain and Inflammation: The First Aid Challenge
Acute injuries present a unique challenge for both clinicians and first responders, as timely intervention directly influences recovery outcomes.
2.1 Understanding Acute Injuries
Acute injuries involve sudden trauma to tissues such as muscles, ligaments, tendons, or joints. Common examples include ankle sprains, wrist ligament tears, muscle strains, and minor contusions. At the molecular level, tissue trauma triggers an inflammatory response characterized by vasodilation, leukocyte migration, increased vascular permeability, and the release of inflammatory mediators. This results in classical symptoms such as pain, swelling, redness, and impaired mobility. Immediate intervention aims to moderate these processes, limit secondary tissue damage, and preserve function.
2.2 Traditional First Aid Methods
Conventional first aid for acute injuries often follows the RICE protocol—Rest, Ice, Compression, and Elevation. Ice packs temporarily reduce tissue temperature, slowing metabolism and limiting edema. Compression and elevation improve venous return and reduce swelling. However, these approaches have limitations: ice packs can be uneven, may cause skin discomfort, and require extended application periods for effectiveness. RICE alone does not actively modulate inflammatory mediators at the cellular level, and its analgesic effects are often slower than desired for rapid pain relief, particularly in high-performance or time-sensitive environments.
2.3 Why Rapid Intervention Matters
Immediate and precise pain and inflammation control can significantly improve recovery trajectories. By reducing edema early, tissue oxygenation is preserved, minimizing hypoxia-induced secondary damage. Quick analgesia also allows early mobilization, which supports optimal alignment of collagen fibers during healing, decreasing the risk of chronic instability or stiffness. For athletes, first responders, and workers in high-risk environments, reducing pain and inflammation within minutes is crucial for continued participation and to prevent escalation into more severe injury stages. CO₂ Cryotherapy addresses these needs effectively, bridging the gap between conventional ice therapy and emergency intervention.
3. CO₂ Cryotherapy in First Aid Applications
CO₂ Cryotherapy can be seamlessly integrated into first aid protocols, offering immediate symptom relief and targeted inflammation control.
3.1 Immediate Pain Relief
When applied to an acute injury, CO₂ Cryotherapy acts directly on nociceptors and sensory nerve endings. The rapid cooling decreases nerve conduction velocity, effectively blocking pain signal transmission to the central nervous system. Additionally, the cold-induced reduction in local metabolic rate and inflammatory mediator activity further diminishes nociceptive stimulation. Clinical observations suggest that many patients report significant pain relief within minutes, which facilitates early functional assessment and safe mobilization. The dry nature of CO₂ application avoids discomfort associated with wet or frozen ice packs, making it particularly useful for sensitive areas such as elbows, knees, and ankles.
3.2 Swelling and Inflammation Control
Acute injuries often trigger localized edema due to increased vascular permeability and plasma exudation. CO₂ Cryotherapy’s vasoconstrictive effect temporarily reduces blood flow to the affected area, limiting additional fluid accumulation. Furthermore, the treatment can modulate pro-inflammatory cytokines such as TNF-α and interleukins, reducing leukocyte recruitment and oxidative stress. Short treatment cycles followed by reactive hyperemia enhance microcirculation and lymphatic drainage, accelerating fluid reabsorption. This dual mechanism—immediate vasoconstriction followed by controlled reperfusion—optimizes inflammation management, reducing swelling and secondary tissue damage.
3.3 Use Cases and Practical Examples
CO₂ Cryotherapy has been applied effectively in a range of first aid scenarios. On the sports field, it is used immediately after ankle sprains or hamstring strains to limit swelling and pain. In workplace incidents, it can be applied to minor contusions or soft tissue trauma to allow safe movement and reduce downtime. For home use, portable CO₂ devices provide localized therapy for acute injuries without the need for large ice packs or medical supervision. Application typically involves holding the CO₂ nozzle 1–2 cm from the skin for 1–3 minutes per affected area, ensuring precise cooling without damaging surrounding tissue.
4. Safety, Contraindications, and Precautions
While CO₂ Cryotherapy is generally safe, proper application is critical to prevent adverse effects and maximize therapeutic benefits.
4.1 Safety Measures
Operators should maintain a safe distance between the nozzle and the skin to avoid frostbite or cold burns. Treatments typically last 1–3 minutes, with intermittent monitoring of patient comfort and skin response. Protective barriers or gloves may be used on sensitive skin or in pediatric and elderly patients. Equipment should be calibrated according to manufacturer specifications, and staff should receive training on safe handling procedures. These measures ensure that CO₂ Cryotherapy remains a rapid, effective, and low-risk first aid intervention.
4.2 Contraindications
CO₂ Cryotherapy should not be used over open wounds, active infections, or areas with impaired circulation. Patients with cardiovascular instability, Raynaud’s phenomenon, or cold hypersensitivity should avoid the treatment. Caution is advised for individuals with neuropathy, as reduced sensation may increase the risk of overexposure. Screening for contraindications before first aid application ensures patient safety and minimizes complications.
4.3 Tips for First-Time Users
For first-time users, starting with shorter exposure times and lower intensity is recommended. Monitoring skin color, temperature, and patient-reported sensations is essential. Educating patients or caregivers about expected sensations—initial cold, mild tingling, and subsequent warmth—improves compliance and comfort. Combining CO₂ Cryotherapy with standard first aid methods enhances results while maintaining safety.
5. Combining CO₂ Cryotherapy with Other First Aid Techniques
CO₂ Cryotherapy is most effective when integrated with established first aid practices and rehabilitation strategies.
5.1 Integration with RICE
Although CO₂ Cryotherapy offers immediate analgesia and inflammation control, pairing it with RICE enhances overall outcomes. After a brief CO₂ session, compression and elevation help stabilize tissue and facilitate fluid reabsorption. Short-term rest following treatment prevents additional stress on the injured area. This combined approach leverages both the physiological benefits of cryotherapy and the mechanical support of traditional first aid.
5.2 Post-Injury Mobility and Rehabilitation
Rapid pain relief from CO₂ Cryotherapy allows clinicians to assess joint mobility and initiate gentle rehabilitation exercises sooner. Early movement prevents joint stiffness, promotes proper collagen alignment, and reduces the risk of chronic functional impairment. In sports or occupational settings, this integration shortens recovery timelines and facilitates safe return to activity, highlighting CO₂ Cryotherapy’s role not only as a first aid tool but also as a bridge to structured rehabilitation programs.
FAQ
How quickly does CO₂ Cryotherapy relieve pain?
Most patients report noticeable analgesia within 2–5 minutes of application.
Is it safe for children or elderly patients?
Yes, with adjusted exposure times and monitored application; always consider skin sensitivity.
Can CO₂ Cryotherapy replace ice packs entirely?
It can complement or replace ice packs for rapid targeted cooling, but integration with RICE is recommended.
How long should a first aid session last?
Typically 1–3 minutes per affected area, repeated as necessary with intervals.
Are there risks of overuse in acute injuries?
Excessive exposure can cause skin irritation or frostbite; follow manufacturer guidelines.
Conclusion
CO₂ Cryotherapy provides a rapid, targeted, and non-invasive option for first aid in acute injuries. By combining immediate pain relief, inflammation control, and enhanced microcirculation, it improves recovery outcomes and patient comfort. While generally safe, proper technique, awareness of contraindications, and integration with traditional first aid methods maximize effectiveness. For athletes, office workers, or individuals at home, CO₂ Cryotherapy represents a practical and evidence-based intervention that bridges the gap between emergency pain management and long-term rehabilitation.
References
Local Cryotherapy. CO₂ Cryotherapy: The First Aid Essential for Fast Pain Management.
Hamblin MR. Mechanisms and applications of the anti-inflammatory effects of photobiomodulation. AIMS Biophysics. 2017;4(3):337–361.
https://www.aimspress.com/article/10.3934/biophy.2017.3.337
Bjordal JM, Johnson MI, Iversen V, et al. Low-level laser therapy in acute pain: a systematic review of possible mechanisms. Journal of Pain. 2006;7(3):219–225.
https://www.jpain.org/article/S1526-5900(06)00587-4/fulltext
Chung H, Dai T, Sharma SK, et al. The nuts and bolts of low-level laser (light) therapy. Annals of Biomedical Engineering. 2012;40(2):516–533.


