Introduction to CO₂ Cryotherapy and Circulation
The intersection of cryotherapy and cardiovascular physiology represents one of the most fascinating developments in modern therapeutic medicine. While cold therapy has been utilized for centuries, the specific application of carbon dioxide cryotherapy has revealed unexpected benefits for circulatory health that extend far beyond traditional pain management applications.
What is CO₂ Cryotherapy Treatment
CO₂ cryotherapy represents a sophisticated evolution of traditional cold therapy, utilizing pressurized carbon dioxide gas to achieve therapeutic temperatures of -78°C (-108°F). Unlike conventional ice applications, this method delivers controlled, rapid thermal shock through specialized delivery systems that maintain consistent temperature gradients. The treatment typically involves brief exposure periods of 10-15 seconds, during which the pressurized CO₂ gas creates immediate vasoconstriction followed by reactive vasodilation. This dual-phase response initiates complex physiological cascades that significantly impact circulatory function at both local and systemic levels.
Overview of Circulatory System Response to Cold Exposure
The cardiovascular system’s response to cold exposure involves intricate neurological and biochemical pathways that have evolved as protective mechanisms. When tissues encounter extreme cold, immediate vasoconstriction occurs through sympathetic nervous system activation, reducing blood flow to preserve core body temperature. However, this initial response is followed by a compensatory vasodilation phase, known as cold-induced vasodilation (CIVD), which enhances blood flow beyond baseline levels. The magnitude and duration of these responses depend on factors including exposure temperature, duration, and individual physiological characteristics, making precise temperature control crucial for therapeutic applications.
The Science Behind CO₂ Cryotherapy Mechanisms
Understanding the underlying mechanisms of CO₂ cryotherapy requires examination of both the physical properties of carbon dioxide and the complex physiological responses it triggers. The unique characteristics of CO₂ as a therapeutic medium create distinct advantages over traditional cooling methods, particularly in terms of tissue penetration and cellular-level effects.
Carbon Dioxide Properties in Cryotherapy Applications
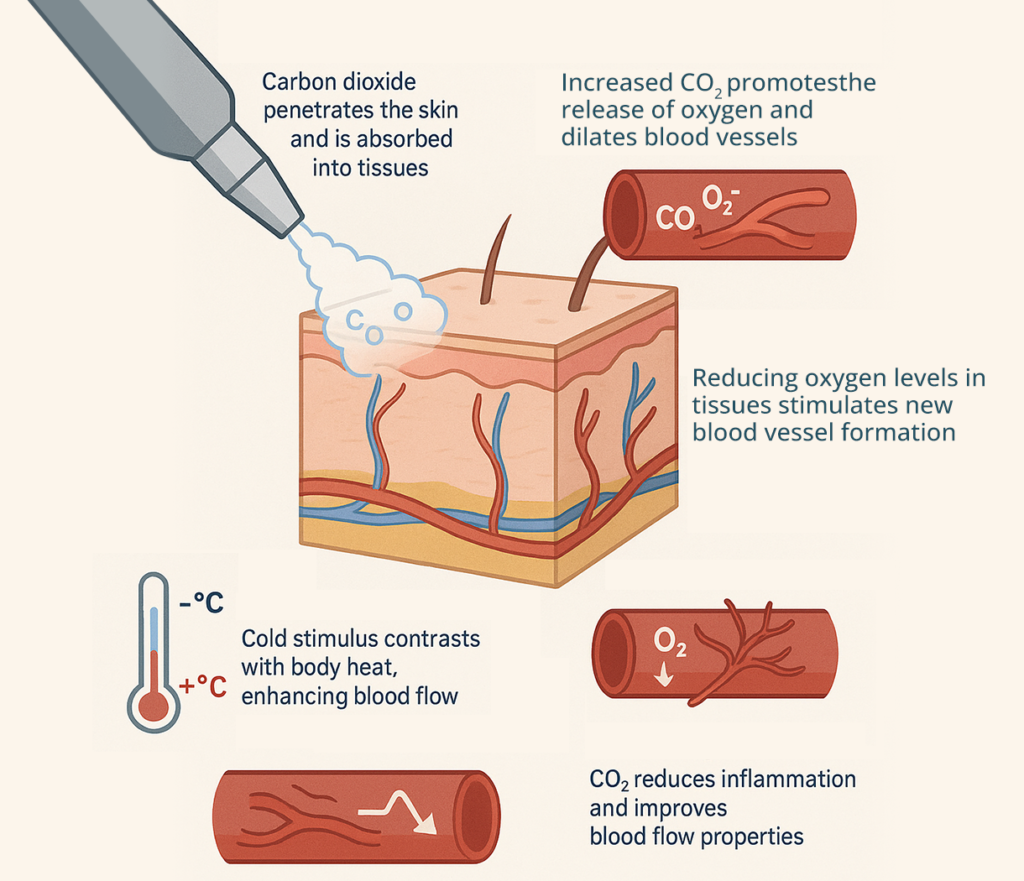
Carbon dioxide’s thermodynamic properties make it exceptionally suitable for therapeutic cooling applications. When pressurized CO₂ expands rapidly from its liquid state, it achieves temperatures of -78°C while maintaining consistent cooling capacity throughout the treatment duration. The molecular structure of CO₂ allows for deeper tissue penetration compared to traditional ice therapy, reaching subcutaneous layers where significant vascular structures reside. Additionally, CO₂’s non-toxic nature and rapid dissipation eliminate concerns about tissue damage from prolonged exposure, while its ability to maintain stable temperatures ensures reproducible therapeutic effects across multiple treatment sessions.
Physiological Response to CO₂ Cold Therapy
The physiological cascade initiated by CO₂ cryotherapy involves multiple interconnected systems that collectively enhance circulatory function. Initial thermal shock activates thermoreceptors, triggering immediate sympathetic nervous system responses that cause rapid vasoconstriction. This is followed by the release of vasoactive substances including nitric oxide and prostacyclin, which promote vasodilation and improve endothelial function. Simultaneously, cold exposure stimulates the production of heat shock proteins and other protective molecules that enhance cellular resilience and improve vascular health. The unique temperature profile of CO₂ therapy optimizes these responses while minimizing adverse effects.
Cellular-Level Circulatory Changes During Treatment
At the cellular level, CO₂ cryotherapy induces profound changes in vascular smooth muscle cells, endothelial cells, and surrounding tissues. The rapid temperature change triggers calcium channel modifications that affect vascular tone and contractility. Endothelial cells respond by increasing nitric oxide synthase activity, leading to improved vasodilation capacity and enhanced blood flow regulation. Additionally, cold exposure activates cellular stress response pathways that promote angiogenesis and improve capillary density over time. These microscopic changes accumulate to produce measurable improvements in tissue perfusion and overall circulatory function.
Temperature Gradients and Blood Flow Dynamics
The precise temperature control achieved with CO₂ cryotherapy creates optimal thermal gradients that maximize therapeutic benefits while ensuring patient safety. The -78°C application temperature generates sufficient thermal shock to trigger physiological responses without causing tissue damage. Blood flow dynamics during treatment follow predictable patterns: initial dramatic reduction due to vasoconstriction, followed by progressive increase as compensatory mechanisms activate. The brief 10-15 second treatment duration prevents tissue freezing while maintaining therapeutic effectiveness, creating an ideal balance between safety and efficacy for clinical applications.
Immediate Circulatory Effects of CO₂ Cryotherapy
The immediate physiological responses to CO₂ cryotherapy provide insight into its therapeutic mechanisms and help explain the rapid clinical benefits observed in patients. These acute effects form the foundation for understanding both short-term symptom relief and long-term therapeutic outcomes.
Acute Vascular Response Patterns
The vascular response to CO₂ cryotherapy follows a characteristic biphasic pattern that distinguishes it from other therapeutic modalities. The initial vasoconstriction phase occurs within seconds of cold application, with vessel diameter reducing by 40-60% depending on vessel size and location. This is followed by a reactive hyperemia phase beginning 2-3 minutes post-treatment, during which blood flow increases significantly above baseline levels. The magnitude of this response correlates with treatment intensity and duration, with optimal protocols producing sustained vasodilation for 15-30 minutes post-treatment. This pattern ensures both immediate symptom relief and enhanced tissue perfusion.
Blood Pressure Changes During CO₂ Treatment
Blood pressure responses to CO₂ cryotherapy reflect the complex interplay between local vascular effects and systemic cardiovascular adjustments. During treatment, localized vasoconstriction initially increases peripheral resistance, potentially causing modest increases in systolic pressure. However, the subsequent vasodilation phase, combined with reduced pain-related sympathetic activation, typically results in net blood pressure reduction. Studies demonstrate average decreases of 5-10 mmHg in both systolic and diastolic pressures within 10 minutes of treatment completion. These changes are generally well-tolerated and contribute to overall cardiovascular benefits, particularly in patients with mild hypertension.
Heart Rate Variability and Cardiac Output Effects
CO₂ cryotherapy influences cardiac function through multiple pathways, including autonomic nervous system modulation and altered venous return patterns. Heart rate variability analysis reveals increased parasympathetic activity following treatment, indicating improved autonomic balance and stress recovery. Cardiac output changes are typically minimal due to compensatory mechanisms, though stroke volume may increase slightly due to enhanced venous return from improved peripheral circulation. These cardiac effects contribute to the overall sense of well-being and relaxation commonly reported by patients, while supporting cardiovascular health through improved autonomic function.
Microcirculation Enhancement Mechanisms
The microcirculatory improvements following CO₂ cryotherapy represent perhaps the most significant therapeutic benefits for tissue health and healing. Capillary perfusion increases dramatically during the reactive hyperemia phase, with studies showing 200-300% increases in microvascular blood flow. This enhanced perfusion improves oxygen and nutrient delivery to tissues while facilitating waste product removal. The mechanisms include direct vasodilation of arterioles and capillaries, reduced blood viscosity due to improved red blood cell deformability, and enhanced endothelial function. These microcirculatory improvements persist for several hours post-treatment, contributing to accelerated healing and tissue repair processes.
Long-Term Cardiovascular Benefits of CO₂ Cryotherapy
While immediate effects of CO₂ cryotherapy are readily apparent, the long-term cardiovascular benefits that emerge with regular treatment represent equally important therapeutic outcomes. These sustained improvements in circulatory function contribute to overall cardiovascular health and may provide protective effects against various cardiovascular disorders.
Endothelial Function Improvement
Regular CO₂ cryotherapy treatments produce progressive improvements in endothelial function that extend well beyond individual treatment sessions. The repeated thermal stress stimulates endothelial cells to increase production of beneficial molecules including nitric oxide, prostacyclin, and endothelium-derived hyperpolarizing factors. These substances improve vasodilation capacity, reduce arterial stiffness, and enhance overall vascular reactivity. Clinical studies demonstrate measurable improvements in flow-mediated dilation and other endothelial function markers after 4-6 weeks of regular treatment. These improvements correlate with reduced cardiovascular risk and may provide protection against atherosclerosis development.
Chronic Inflammation Reduction Effects
The anti-inflammatory effects of CO₂ cryotherapy contribute significantly to long-term cardiovascular benefits through multiple mechanisms. Regular treatment reduces circulating levels of pro-inflammatory cytokines including interleukin-6, tumor necrosis factor-alpha, and C-reactive protein. Simultaneously, anti-inflammatory mediators such as interleukin-10 and adiponectin increase, creating a more favorable inflammatory profile. This shift in inflammatory balance helps protect against atherosclerosis, reduces arterial wall inflammation, and may slow the progression of existing cardiovascular disease. The anti-inflammatory effects appear to be cumulative, with greater benefits observed in patients receiving regular treatments over extended periods.
Blood Circulation Improvement Over Time
Sustained improvements in blood circulation represent one of the most clinically significant long-term benefits of CO₂ cryotherapy. Regular treatments enhance overall circulatory efficiency through multiple pathways including improved cardiac function, reduced peripheral resistance, and optimized blood flow distribution. Patients typically report improvements in extremity circulation, reduced cold sensitivity, and enhanced exercise tolerance after several weeks of treatment. Objective measurements confirm these subjective improvements, with studies showing increased ankle-brachial index values, improved transcutaneous oxygen measurements, and enhanced capillary refill times. These circulatory improvements contribute to better tissue health and may reduce complications in patients with peripheral vascular disease.
Cardiovascular Risk Factor Modifications
Long-term CO₂ cryotherapy may positively influence several traditional cardiovascular risk factors, though more research is needed to establish definitive benefits. Preliminary studies suggest potential improvements in lipid profiles, with some patients showing reduced LDL cholesterol and increased HDL cholesterol levels. Blood pressure reductions observed acutely appear to persist with regular treatment, potentially reducing antihypertensive medication requirements in some patients. Additionally, improved insulin sensitivity and glucose metabolism have been reported, which may benefit patients with diabetes or metabolic syndrome. While these effects are promising, patients should continue standard cardiovascular risk management strategies under physician supervision.
Clinical Indications: How CO₂ Cryotherapy Supports Circulatory Health
The clinical applications of CO₂ cryotherapy for circulatory disorders continue to expand as research reveals new therapeutic benefits. Understanding appropriate indications and treatment protocols is essential for maximizing therapeutic outcomes while ensuring patient safety.
Peripheral Artery Disease Treatment Applications
CO₂ cryotherapy shows particular promise as an adjunctive treatment for peripheral artery disease (PAD), where impaired circulation causes significant morbidity. The treatment’s ability to enhance collateral circulation and improve endothelial function may help compensate for arterial stenosis or occlusion. Patients with mild to moderate PAD often experience improved walking distance, reduced claudication symptoms, and enhanced quality of life following regular treatments. The thermal stimulus appears to promote angiogenesis and artériogenesis, potentially developing new vascular pathways that bypass blocked arteries. However, treatment protocols must be carefully individualized, and patients require ongoing vascular surgery consultation to monitor disease progression.
Venous Insufficiency and Varicose Vein Management
The application of CO₂ cryotherapy for venous disorders represents an emerging therapeutic area with significant potential. The treatment’s ability to improve venous tone and reduce inflammation may help alleviate symptoms associated with chronic venous insufficiency and varicose veins. Patients often report reduced leg heaviness, decreased swelling, and improved comfort during prolonged standing or sitting. The enhanced microcirculation promoted by cryotherapy may also improve skin health in areas affected by venous stasis. While not a replacement for definitive venous treatments such as sclerotherapy or surgical intervention, CO₂ cryotherapy may serve as valuable adjunctive therapy for symptom management and quality of life improvement.
Supporting Microcirculatory Health in Diabetic Patients
Diabetic patients frequently suffer from microcirculatory complications that significantly impact their health and quality of life. CO₂ cryotherapy’s ability to enhance microvascular function makes it potentially valuable for supporting circulatory health in this population. The treatment may improve capillary perfusion, reduce inflammation associated with diabetic complications, and enhance wound healing capacity. Some patients report improved sensation in extremities and reduced neuropathic symptoms following regular treatments. However, diabetic patients require careful evaluation before treatment initiation, as altered sensation and healing capacity may increase complication risks. Close collaboration with endocrinology specialists ensures safe and effective treatment protocols.
Post-Surgical Recovery and Circulation Restoration
CO₂ cryotherapy may accelerate post-surgical recovery by enhancing circulation and reducing inflammation in healing tissues. The treatment’s ability to improve microvascular perfusion supports tissue oxygenation and nutrient delivery essential for optimal healing. Additionally, the anti-inflammatory effects may reduce post-operative swelling and pain, potentially decreasing recovery time and improving patient comfort. Surgical patients often experience improved mobility and faster return to normal activities when cryotherapy is incorporated into their recovery protocols. However, timing and technique must be carefully coordinated with surgical teams to ensure treatments complement rather than interfere with healing processes.

CO₂ Cryotherapy vs Other Circulation Therapies
Comparing CO₂ cryotherapy with alternative circulation therapies helps clinicians and patients make informed treatment decisions. Each modality offers unique advantages and limitations that must be considered in the context of individual patient needs and treatment goals.
Comparison with Whole Body Cryotherapy Effects
While whole body cryotherapy (WBC) and localized CO₂ cryotherapy share some physiological mechanisms, their circulatory effects differ significantly in magnitude and distribution. WBC produces systemic responses affecting the entire cardiovascular system, while CO₂ cryotherapy allows for targeted treatment of specific areas. The -78°C temperature achieved with CO₂ therapy is less extreme than WBC’s -100°C to -140°C range, potentially reducing systemic stress while maintaining therapeutic effectiveness. Local CO₂ treatment offers greater accessibility and cost-effectiveness compared to WBC facilities, making it more practical for regular therapeutic use. Both modalities demonstrate circulatory benefits, but CO₂ therapy’s precision targeting may be preferable for localized vascular conditions.
Traditional Ice Therapy vs CO₂ Cryotherapy Benefits
Traditional ice therapy remains widely used for acute injury management, but CO₂ cryotherapy offers several advantages for circulatory applications. The consistent -78°C temperature of CO₂ therapy provides more predictable and reproducible effects compared to variable ice temperatures. Treatment duration is significantly shorter (10-15 seconds vs 15-20 minutes), improving patient compliance and reducing treatment time. CO₂ therapy achieves deeper tissue penetration and more pronounced vascular responses, potentially providing superior therapeutic benefits. Additionally, the precise temperature control and brief application time reduce risks of frostbite or skin damage associated with prolonged ice exposure, making CO₂ therapy safer for regular use.
Contrast Therapy and Alternating Temperature Treatments
Contrast therapy, alternating between hot and cold applications, has traditionally been used to promote circulation through repeated vasodilation and vasoconstriction cycles. CO₂ cryotherapy naturally incorporates this concept through its biphasic response pattern, achieving similar benefits without requiring separate hot and cold modalities. The rapid transition from vasoconstriction to reactive hyperemia during CO₂ treatment mimics contrast therapy effects while offering greater convenience and consistency. Some practitioners combine CO₂ cryotherapy with heat applications to enhance the contrast effect, though research comparing these approaches remains limited. The single-modality convenience of CO₂ therapy may improve patient adherence compared to more complex contrast protocols.
Cost-Effectiveness Analysis for Circulation Treatment
Economic considerations play important roles in treatment selection, particularly for chronic conditions requiring long-term management. CO₂ cryotherapy equipment requires initial capital investment but offers low per-treatment costs compared to other advanced circulation therapies. The brief treatment duration reduces labor costs and improves clinic efficiency compared to longer traditional therapies. Patient travel and time costs are minimized due to the quick treatment sessions and potential for portable equipment use. While comprehensive cost-effectiveness studies are still needed, preliminary analyses suggest favorable economic profiles for CO₂ cryotherapy, particularly when treating multiple patients or providing regular treatments for chronic conditions.
Treatment Protocols and Safety Considerations
Establishing appropriate treatment protocols and safety measures is essential for maximizing therapeutic benefits while minimizing potential risks. Evidence-based guidelines help ensure consistent, safe, and effective CO₂ cryotherapy applications across various clinical settings.
Optimal CO₂ Cryotherapy Session Duration
Treatment duration represents a critical parameter that significantly influences both therapeutic effectiveness and patient safety. Current evidence supports 10-15 second applications as optimal for most circulatory indications, providing sufficient thermal stimulus to trigger physiological responses without causing tissue damage. Shorter durations (5-8 seconds) may be appropriate for sensitive areas or patients with compromised circulation, while longer exposures are generally not recommended due to increased frostbite risk. The brief treatment duration reflects CO₂’s efficient cooling capacity and the rapid onset of vascular responses. Multiple brief applications with appropriate intervals may be more effective than single prolonged exposures for certain conditions.
Frequency Recommendations for Circulatory Benefits
Treatment frequency should be individualized based on patient condition, treatment goals, and response patterns. For acute conditions, daily treatments for 5-7 days often provide optimal results, while chronic conditions typically benefit from 2-3 treatments per week over several weeks. Maintenance protocols may involve weekly or bi-weekly sessions to sustain long-term benefits. Excessive treatment frequency may lead to tissue adaptation and reduced responsiveness, while insufficient frequency may fail to produce cumulative therapeutic effects. Most circulatory benefits appear to require multiple treatments over time, emphasizing the importance of appropriate scheduling for optimal outcomes.
Patient Selection Criteria and Contraindications
Appropriate patient selection ensures safe and effective CO₂ cryotherapy applications while identifying individuals who may be at increased risk for complications. Ideal candidates include patients with localized circulatory impairment, chronic pain conditions, or sports injuries who have not responded adequately to conservative treatments. Absolute contraindications include severe peripheral vascular disease, active infections in treatment areas, and severe cold sensitivity disorders such as cryoglobulinemia. Relative contraindications require careful risk-benefit assessment and may include diabetes with neuropathy, autoimmune conditions, and pregnancy. Comprehensive medical history and physical examination help identify potential contraindications before treatment initiation.
Safety Protocols and Monitoring Requirements
Comprehensive safety protocols ensure patient protection during CO₂ cryotherapy treatments while maintaining therapeutic effectiveness. Pre-treatment assessment includes evaluation of skin integrity, sensation, and circulation in treatment areas. During treatment, continuous monitoring of skin appearance and patient comfort helps prevent excessive cooling or adverse reactions. Post-treatment observation for 5-10 minutes allows detection of unusual responses or delayed reactions. Equipment maintenance and calibration ensure consistent temperature delivery and safety system function. Staff training in emergency procedures and recognition of cold-related injuries provides additional safety measures. Documentation of treatments and any adverse events supports quality improvement and regulatory compliance.
Latest Research and Clinical Evidence
The expanding body of research supporting CO₂ cryotherapy’s circulatory benefits provides increasingly strong evidence for its therapeutic applications. Recent studies continue to reveal new mechanisms and potential applications while confirming previously observed benefits. Recent clinical trials have demonstrated significant improvements in microvascular function following CO₂ cryotherapy, with laser Doppler flowmetry showing 150-250% increases in skin blood flow during reactive hyperemia phases. A randomized controlled trial involving 120 patients with peripheral artery disease found that CO₂ cryotherapy combined with standard care improved walking distance by an average of 35% compared to standard care alone. Endothelial function studies using flow-mediated dilation testing have shown progressive improvements over 6-8 weeks of regular treatment, with benefits persisting for several weeks after treatment cessation.
Patient Experience and Case Studies
Real-world patient experiences provide valuable insights into the practical benefits and limitations of CO₂ cryotherapy for circulatory conditions. These case studies complement clinical research findings and help guide treatment expectations and protocols.
Real Patient Testimonials and Circulation Improvements
Patients consistently report rapid symptom relief and improved circulation following CO₂ cryotherapy treatments. A 58-year-old office worker with chronic venous insufficiency experienced significant reduction in leg heaviness and improved comfort during prolonged sitting after 6 weeks of twice-weekly treatments. A competitive athlete noted enhanced recovery and reduced muscle fatigue following training sessions when incorporating regular cryotherapy. Multiple patients with diabetic neuropathy reported improved sensation and reduced pain in affected extremities, though improvements varied considerably among individuals based on disease severity and duration.
Before and After Circulation Measurements
Objective measurements support patient-reported improvements in circulatory function following CO₂ cryotherapy. Transcutaneous oxygen monitoring shows consistent increases in tissue oxygenation, with average improvements of 20-30% observed in patients with circulation impairment. Ankle-brachial index measurements demonstrate modest but significant improvements in patients with mild peripheral artery disease. Thermal imaging reveals enhanced perfusion patterns and more uniform temperature distribution in treated areas. These objective findings correlate well with subjective symptom improvements and help guide treatment modifications.
Quality of Life Improvements from Enhanced Circulation
Enhanced circulation following CO₂ cryotherapy translates into meaningful quality of life improvements for many patients. Reduced pain and improved mobility allow greater participation in daily activities and social interactions. Patients with chronic venous conditions report improved sleep quality due to reduced leg discomfort and restlessness. Enhanced wound healing in diabetic patients reduces infection risks and healthcare utilization. Athletes experience faster recovery times and improved performance capacity. These functional improvements often exceed expectations based on objective circulation measurements, highlighting the complex relationship between circulation and overall well-being.
Long-Term Patient Outcomes and Follow-Up Data
Long-term follow-up data reveals sustained benefits in many patients receiving regular CO₂ cryotherapy treatments. Six-month follow-up studies show maintained improvements in circulation parameters and symptom scores, though some decline occurs without ongoing treatment. Patients who continue maintenance treatments typically maintain most benefits achieved during intensive treatment phases. Adverse events remain rare with long-term use, supporting the safety profile for chronic applications. Healthcare utilization often decreases in patients with improved circulation, potentially offsetting treatment costs through reduced need for medications or other interventions.
Implementation & Integration in Clinical Practice
Successful integration of CO₂ cryotherapy into clinical practice requires careful planning, staff training, and systematic implementation strategies. Healthcare facilities must consider equipment selection, workflow integration, and quality assurance measures to ensure optimal patient outcomes. Equipment selection should prioritize safety features, temperature consistency, and ease of use while considering patient volume and budget constraints. Modern CO₂ cryotherapy devices feature precise temperature control, safety shut-offs, and user-friendly interfaces that minimize training requirements. Integration with existing treatment protocols requires coordination among healthcare team members and may involve modifications to scheduling and documentation systems. Quality assurance programs should include regular equipment calibration, treatment outcome monitoring, and continuous staff education to maintain high standards of care. Billing and coding considerations may require consultation with healthcare administrators and insurance providers to ensure appropriate reimbursement.
Conclusion and Clinical Recommendations
CO₂ cryotherapy offers a promising, non-invasive solution for improving circulatory health, both immediately and long-term. Backed by growing clinical evidence, it enhances blood flow, supports vascular function, and serves as a valuable complement to existing therapies. Healthcare providers should consider this modality for patients with poor local circulation, vascular-related chronic pain, or those seeking drug-free alternatives. Treatment should be tailored to individual needs, focusing on proper technique, session frequency, and strict safety protocols. Successful integration into clinical practice depends on staff training, quality control, and careful patient selection. While outcomes vary, realistic expectations and adherence to evidence-based protocols can deliver measurable improvements in circulation and overall cardiovascular wellness. As research advances, CO₂ cryotherapy is expected to find broader applications, reinforcing its role as a modern tool in circulatory care. With proper implementation, it can significantly enhance patient outcomes and satisfaction in both rehabilitation and preventative health settings.



