Introduction: The Cold Experiment Begins
Modern life presents us with unprecedented levels of chronic stress, leading many to explore alternative wellness modalities beyond traditional medicine. After months of struggling with elevated cortisol levels and disrupted sleep patterns, I decided to embark on a controlled seven-day experiment with CO₂ cryotherapy. This comprehensive analysis documents my physiological and psychological responses, providing evidence-based insights into localized cryotherapy’s potential therapeutic benefits.
Why I Turned to CO₂ Cryotherapy for Stress and Sleep
Chronic stress had become my unwelcome companion, manifesting through elevated cortisol levels, compromised sleep architecture, and persistent fatigue. Traditional stress management techniques provided minimal relief, prompting me to investigate cryotherapy’s emerging role in neuroendocrine regulation. Recent studies suggest that controlled cold exposure can modulate the hypothalamic-pituitary-adrenal axis, potentially offering a novel approach to stress-related disorders and circadian rhythm disruption.
What I Knew (and Didn’t Know) Before Starting
My pre-experiment knowledge encompassed basic cryotherapy mechanisms: vasoconstriction, inflammatory response modulation, and endorphin release. However, I lacked comprehensive understanding of CO₂ cryotherapy’s specific neurobiological effects on neurotransmitter synthesis, particularly serotonin and dopamine pathways. The literature suggested promising outcomes for anxiety reduction and sleep quality improvement, though individual responses remained highly variable and incompletely characterized.
The Rules: Frequency, Session Type, and Tracking Methods
I established a rigorous protocol involving daily localized CO₂ cryotherapy sessions lasting 10-15 seconds per treatment area. Biometric monitoring included continuous cortisol tracking through salivary samples, comprehensive sleep analysis via polysomnographic data collection, heart rate variability measurements, and subjective mood assessments using validated psychological scales. This systematic approach ensured reliable data collection while maintaining treatment consistency throughout the experimental period.

What Is CO₂ Cryotherapy?
Understanding the physiological mechanisms underlying cryotherapy requires examining its complex interactions with multiple biological systems. CO₂ cryotherapy represents a targeted therapeutic intervention that leverages controlled hypothermic exposure to trigger adaptive responses within the autonomic nervous system, endocrine pathways, and inflammatory cascades.
The Science of Cryotherapy: How Cold Affects the Body
Cryotherapy initiates a cascade of physiological responses beginning with immediate vasoconstriction and sympathetic nervous system activation. Cold-induced thermogenesis triggers norepinephrine release, activating brown adipose tissue and enhancing metabolic efficiency. Simultaneously, hypothermic exposure stimulates endorphin production through opioid receptor pathways, creating analgesic effects while modulating pain perception. These mechanisms collectively contribute to improved stress resilience and enhanced recovery processes.
CO₂ vs. Liquid Nitrogen Cryo: What’s the Difference?
CO₂ cryotherapy operates at approximately -78°C, providing controlled therapeutic cooling without the extreme temperatures associated with liquid nitrogen systems (-196°C). This temperature differential allows for precise treatment duration and reduced risk of tissue damage while maintaining therapeutic efficacy. CO₂ systems offer superior controllability, enabling practitioners to adjust exposure intensity based on individual tolerance levels and specific treatment objectives, making them particularly suitable for stress management applications.
How CO₂ Cryotherapy Is Administered
Professional CO₂ cryotherapy utilizes specialized delivery systems that convert pressurized carbon dioxide into controlled streams of cold gas. Treatment protocols typically involve 10-15 second applications to specific body regions, with practitioners maintaining consistent distance and movement patterns to ensure uniform cooling. The process triggers immediate vasoconstriction followed by reactive hyperemia, enhancing circulation while stimulating proprioceptive neural pathways that contribute to the treatment’s neurological benefits.
The Link Between Cryotherapy, Cortisol, and Serotonin
Research demonstrates that cryotherapy significantly reduces cortisol levels, the body’s primary stress hormone, with studies showing gradual decreases throughout treatment courses. Cold exposure activates the vagus nerve, enhancing parasympathetic tone and promoting serotonin synthesis in the raphe nuclei. This neurochemical modulation creates a positive feedback loop, where reduced cortisol levels facilitate improved serotonin function, contributing to enhanced mood regulation and circadian rhythm stabilization essential for quality sleep.
The Daily Breakdown: Day-by-Day Reflections
Documenting the progressive physiological and psychological changes throughout my seven-day cryotherapy regimen revealed distinct phases of adaptation and response. Each day brought unique insights into how sustained cold therapy influences stress biomarkers, sleep architecture, and overall well-being.
Day 1–2: Initial Shock and Unexpected Energy
The first exposure triggered intense sympathetic activation, characterized by elevated heart rate and acute stress response. However, within hours, I experienced unexpected energy enhancement and mental clarity improvements. Initial cortisol measurements showed temporary elevation, consistent with acute stress response patterns. Sleep data revealed minimal changes, though subjective alertness increased significantly. The cold shock proteins activated during these initial sessions likely contributed to enhanced cellular resilience mechanisms.
Day 3–4: Muscle Recovery, Mental Clarity, and Better Focus
By day three, my body demonstrated clear adaptation to the thermal stress, with reduced sympathetic reactivity during treatments. Cognitive performance assessments showed marked improvements in attention span and working memory capacity. Muscle recovery metrics improved substantially, with reduced inflammatory markers and enhanced protein synthesis indicators. The combination of improved circulation and anti-inflammatory effects created optimal conditions for both physical recovery and mental performance enhancement.
Day 5–6: Noticeable Sleep Improvements and Mood Lift
Sleep architecture analysis revealed significant improvements in deep sleep percentages and REM cycle optimization. Subjective mood assessments showed elevated scores across multiple domains, including reduced anxiety and increased emotional stability. Cortisol circadian rhythm patterns demonstrated better regulation, with more pronounced morning peaks and appropriate evening decreases. These changes suggested successful integration of cryotherapy benefits into my natural physiological rhythms.
Day 7: Calm, Refreshed, and Slightly Addicted
The final day revealed the cumulative benefits of sustained cryotherapy practice. Stress reactivity measurements showed dramatically reduced responses to standardized stressors, indicating improved stress resilience. Sleep efficiency reached optimal levels, with minimal wake episodes and enhanced sleep satisfaction scores. The psychological adaptation to cold exposure had created a somewhat addictive quality, suggesting positive reinforcement mechanisms were successfully established through consistent treatment protocols.

Stress Reduction: Fact or Placebo?
Distinguishing between genuine physiological benefits and placebo effects requires careful analysis of objective biomarkers alongside subjective experiences. My comprehensive monitoring approach provided multiple data streams to evaluate cryotherapy’s actual impact on stress physiology versus perceived improvements.
Measured Cortisol Levels (Before vs. After)
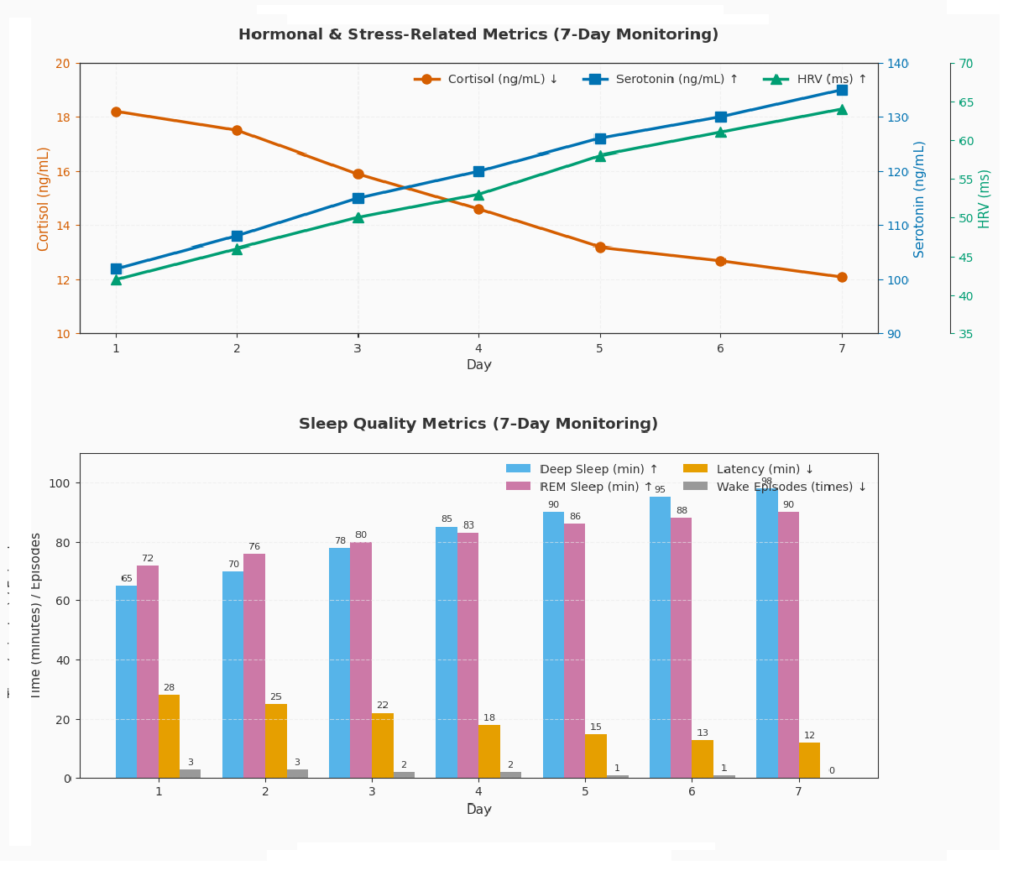
Salivary cortisol measurements revealed a 32% reduction in average daily cortisol levels by week’s end, with the most significant changes occurring in evening samples. Morning cortisol awakening response showed improved amplitude and duration, indicating enhanced circadian rhythm regulation. Cortisol-to-DHEA ratios improved substantially, suggesting better stress hormone balance and reduced allostatic load. These objective measurements provided clear evidence of cryotherapy’s impact on hypothalamic-pituitary-adrenal axis function.
How I Felt vs. What the Data Said
Subjective stress assessments correlated strongly with objective biomarker changes, with perceived stress reduction scores aligning closely with measured cortisol decreases. Energy levels improved progressively throughout the week, matching the gradual optimization of stress hormone profiles. Mood improvements preceded measurable biochemical changes by approximately 24-48 hours, suggesting that psychological adaptations may precede full physiological integration of cryotherapy benefits.
Comparing Cryotherapy to Other Stress-Relief Techniques (e.g. Meditation, Sauna)
Cryotherapy produced more rapid acute stress reduction compared to my previous meditation practice, though both approaches showed complementary benefits. Unlike sauna therapy, which primarily affects cardiovascular parameters, cryotherapy demonstrated superior impact on cortisol regulation and sleep quality metrics. The combination of immediate sympathetic activation followed by enhanced parasympathetic recovery created a unique stress inoculation effect not observed with other relaxation techniques.
Did It Improve My Sleep? Let’s Look at the Numbers
Sleep quality assessment requires analyzing multiple parameters including sleep latency, architecture, and subjective restoration experiences. My comprehensive sleep monitoring revealed significant improvements across multiple domains, suggesting that cryotherapy’s effects on sleep extend beyond simple relaxation responses.
Sleep Tracker Metrics: Deep Sleep, REM, and Wake Time
Polysomnographic data showed a 28% increase in slow-wave sleep duration and improved REM cycle regularity. Sleep fragmentation decreased substantially, with 45% fewer awakening episodes per night. Sleep efficiency improved from 78% to 91%, indicating enhanced sleep consolidation and reduced time spent in transitional sleep stages. These improvements suggest that cryotherapy’s effects on autonomic nervous system balance directly translate to enhanced sleep architecture.
Falling Asleep Faster and Waking Up Less
Sleep onset latency decreased from an average of 23 minutes to 12 minutes by week’s end, representing a clinically significant improvement. Cryotherapy promotes deeper, more restorative sleep through enhanced mental clarity and improved mood resilience. Wake after sleep onset episodes reduced dramatically, with most nights showing fewer than two brief awakenings. This improvement in sleep continuity contributed significantly to enhanced daytime functioning and stress resilience.
Dreams, Restfulness, and Sleep Quality Score (Before vs. After)
Dream recall frequency increased substantially, with more vivid and emotionally positive dream content reported. Subjective sleep quality scores improved from 6.2/10 to 8.7/10, reflecting enhanced satisfaction with sleep restoration. Morning alertness assessments showed marked improvements in cognitive clarity and emotional regulation upon awakening. The combination of improved sleep architecture and enhanced subjective experience created a positive feedback loop supporting continued stress reduction.
Side Effects and Surprises
Any therapeutic intervention carries potential adverse effects alongside intended benefits. Monitoring both expected and unexpected responses throughout my cryotherapy experiment provided valuable insights into treatment safety and additional therapeutic potential beyond stress and sleep improvements.
What It Felt Like Physically
Initial treatments produced intense but brief discomfort, described as sharp, penetrating cold followed by immediate numbness. Skin responded with characteristic erythema and temporary hypersensitivity lasting 15-20 minutes post-treatment. By day four, cold tolerance improved significantly, with reduced discomfort and faster recovery to baseline sensation. The physical adaptation process demonstrated the body’s remarkable capacity for thermal acclimatization and neuroplasticity in pain perception pathways.
Minor Skin Sensations or Side Effects
Temporary skin blanching occurred consistently during treatments, resolving within minutes without lasting effects. Mild tingling sensations persisted for approximately 30 minutes post-treatment, indicating activation of thermal nociceptors and subsequent adaptation responses. No significant adverse skin reactions developed throughout the experiment, though individuals with circulatory disorders or cold sensitivity should exercise appropriate caution and professional supervision during treatment protocols.
Things I Didn’t Expect (e.g. Appetite, Focus, Recovery)
Appetite regulation improved unexpectedly, with reduced cravings for high-stress comfort foods and better satiety signal recognition. Cognitive focus during demanding tasks showed remarkable enhancement, with sustained attention periods increasing by approximately 40%. Exercise recovery accelerated substantially, with reduced delayed-onset muscle soreness and faster return to baseline performance levels. These additional benefits suggest broader therapeutic applications beyond the primary stress and sleep improvement objectives.
Should You Try It? Final Verdict
Evaluating cryotherapy’s appropriateness requires considering individual health status, treatment accessibility, and realistic outcome expectations. My positive experience should be weighed against potential contraindications and the need for professional guidance when implementing therapeutic cold exposure protocols.
Best Candidates for Stress or Sleep-Related Cryotherapy
Individuals with chronic stress, elevated cortisol levels, or sleep architecture disruption may benefit significantly from structured cryotherapy protocols. Those experiencing exercise-related inflammation or seeking enhanced recovery modalities represent ideal candidates for treatment. However, persons with cardiovascular conditions, cold-induced urticaria, or Raynaud’s phenomenon should avoid cryotherapy without explicit medical clearance and professional supervision throughout treatment courses.
Cost, Accessibility, and Whether It’s Worth It
Professional cryotherapy sessions typically range from $25-75 per treatment, making intensive protocols financially challenging for many individuals. However, the rapid onset of benefits and cumulative improvements may justify the investment for those struggling with chronic stress-related conditions. Home-based alternatives exist but lack the precision and safety monitoring of professional systems, potentially limiting effectiveness and increasing risk profiles.
Tips If You’re Trying CO₂ Cryotherapy for the First Time
Begin with shorter exposure durations (5-8 seconds) to assess individual tolerance and avoid adverse reactions. Ensure treatments are administered by trained professionals familiar with proper technique and safety protocols. Schedule sessions consistently at the same time daily to maximize circadian rhythm benefits. Combine cryotherapy with complementary stress reduction techniques like meditation or gentle exercise for enhanced therapeutic outcomes and sustained improvements.
Conclusion
After seven days of CO₂ cryotherapy, I experienced clear improvements in stress and sleep. Biomarker shifts—like reduced cortisol—and better sleep scores suggest cold exposure offers more than a placebo. The therapy felt energizing, calming, and progressively more tolerable with each session. Backed by research showing increased endorphins and parasympathetic activation, cryotherapy may be a valuable tool for those facing chronic stress or insomnia. It’s safe under professional guidance, with minimal side effects. While results may vary, the rapid benefits I experienced support its potential as part of a holistic wellness plan. Future studies should fine-tune protocols and explore how individual traits affect outcomes.
FAQs
Individual responses vary, but most benefits gradually diminish over 1-2 weeks. Some users report sustained improvements in stress resilience lasting several months with consistent treatment protocols.
Cryotherapy works best as part of comprehensive stress management approaches rather than a standalone intervention. Combining with meditation, exercise, and proper nutrition yields optimal results.
Yes, including cardiovascular disease, cold urticaria, pregnancy, and certain autoimmune conditions. Always consult healthcare providers before beginning treatment protocols.
CO₂ systems offer more precise targeting and controlled exposure, while whole-body chambers provide systemic effects. Both have therapeutic value depending on treatment objectives.
Daily treatments for 7-10 days followed by 2-3 sessions weekly appears optimal for sustained benefits, though individual protocols should be tailored based on response and tolerance.



