Introduction
The human vascular system operates as a sophisticated network of highways, constantly adjusting traffic flow to meet the body’s ever-changing demands. Among the most fascinating aspects of vascular physiology is the dynamic interplay between vasoconstriction and vasodilation—a process that resembles a physiological rollercoaster. This intricate dance of blood vessel constriction and expansion forms the foundation of how our bodies respond to injury, inflammation, and therapeutic interventions. CO₂ cryotherapy has emerged as a revolutionary treatment modality that harnesses this natural vascular cycling mechanism. By applying controlled cold temperatures of -78°C for precise durations of 10-15 seconds, this therapy triggers a cascade of vascular responses that promote healing, reduce inflammation, and accelerate recovery. Understanding the science behind this “vascular rollercoaster” provides crucial insights into why cryotherapy has become an indispensable tool in modern rehabilitative medicine and sports performance optimization.
The Physiology Behind Vasoconstriction and Vasodilation
The vascular system’s ability to rapidly adjust blood flow represents one of the most elegant examples of physiological homeostasis. This section explores the intricate mechanisms that govern blood vessel diameter changes and their profound impact on tissue health and recovery.
Vasoconstriction: The First Line of Defense
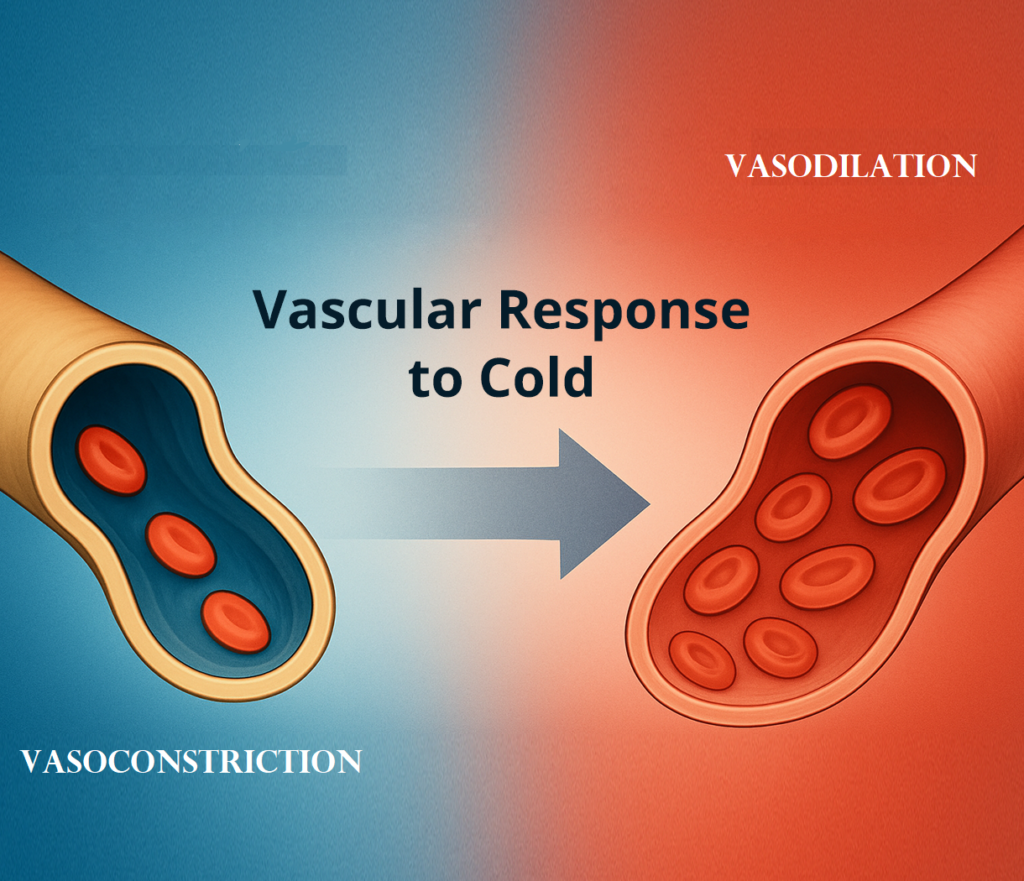
Vasoconstriction occurs when smooth muscle cells surrounding blood vessels contract, reducing the internal diameter of arterioles and capillaries. This immediate response serves as the body’s primary protective mechanism against tissue damage. During cold exposure, sympathetic nerve terminals release norepinephrine, which binds to α-adrenergic receptors on vascular smooth muscle. Initial vasoconstriction within the first 20 minutes of cryotherapy is achieved via activation of post-synaptic α-adrenergic receptors. The process also involves endothelin-1 release from endothelial cells, creating a powerful vasoconstrictor effect that minimizes blood loss and reduces metabolic demands in stressed tissues.
Vasodilation: The Rebound Phase
Following the initial constrictive phase, vasodilation represents the body’s healing response characterized by smooth muscle relaxation and increased vessel diameter. This process involves multiple molecular pathways, including nitric oxide (NO) release from endothelial cells, prostacyclin production, and adenosine accumulation. The vasodilatory response facilitates enhanced nutrient delivery, waste product removal, and immune cell recruitment to affected tissues. Vasodilation can be induced by cold after an initial period of vasoconstriction if the cold exposure lasts for more than approximately 15 minutes. This rebound effect creates the therapeutic window that makes cryotherapy particularly effective for tissue repair and inflammation management.
Why the Body Alternates Between the Two
The alternation between vasoconstriction and vasodilation serves multiple physiological purposes beyond simple temperature regulation. This biphasic response optimizes tissue perfusion while protecting against excessive inflammatory responses. During the constrictive phase, reduced blood flow limits the influx of inflammatory mediators and prevents tissue edema. The subsequent dilatory phase ensures adequate oxygen and nutrient supply for cellular repair processes. This cycling mechanism also enhances lymphatic drainage, facilitating the removal of metabolic waste products and inflammatory debris that accumulate during tissue stress or injury.
Key Terms in Vascular Dynamics
Understanding vascular dynamics requires familiarity with several critical physiological concepts that govern blood flow regulation and tissue perfusion responses.
Reactive Hyperemia
Reactive hyperemia represents the magnitude of limb reperfusion following a brief period of ischemia induced by arterial occlusion. This phenomenon occurs when blood flow is temporarily restricted and then restored, resulting in a compensatory increase in perfusion that exceeds baseline levels. In cryotherapy applications, reactive hyperemia manifests as the enhanced blood flow that follows the initial vasoconstrictor response. This mechanism is crucial for delivering therapeutic benefits, as it ensures that tissues receive an abundance of oxygen, nutrients, and immune factors necessary for optimal healing and recovery.
Microcirculation
Microcirculation encompasses the network of smallest blood vessels, including arterioles, capillaries, and venules, with diameters typically less than 100 micrometers. These vessels are the primary sites of nutrient and gas exchange between blood and tissues. Microcirculatory function is particularly sensitive to temperature changes and represents the primary target of cryotherapy interventions. The health of microcirculation directly impacts tissue oxygenation, waste removal, and inflammatory responses. Dysfunction in microcirculatory networks often underlies chronic pain conditions, delayed healing, and persistent inflammation that cryotherapy can effectively address.
Endothelial Function
Endothelial cells form the inner lining of blood vessels and serve as the interface between circulating blood and vessel walls. These cells produce numerous vasoactive substances, including nitric oxide, prostacyclin, and endothelin, which regulate vascular tone and blood flow. Endothelial dysfunction contributes to various pathological conditions, including atherosclerosis, hypertension, and chronic inflammatory diseases. Cryotherapy can positively influence endothelial function by reducing oxidative stress, modulating inflammatory signaling pathways, and promoting the release of beneficial vasoactive compounds that support vascular health and tissue repair mechanisms.
How CO₂ Cryotherapy Triggers Vascular Cycling
CO₂ cryotherapy represents a sophisticated approach to therapeutic cooling that leverages the unique properties of carbon dioxide to create controlled vascular responses. This section examines the specific mechanisms through which CO₂-based cooling systems generate therapeutic vascular cycling.
Rapid Cooling via CO₂ Spray Technology
CO₂ cryotherapy systems utilize the sublimation properties of solid carbon dioxide to achieve rapid tissue cooling. When pressurized liquid CO₂ is released through specialized nozzles, it undergoes immediate phase transition, creating temperatures of -78°C at the point of application. This extreme cold exposure triggers immediate vasoconstriction through multiple mechanisms: direct smooth muscle contraction, sympathetic nervous system activation, and release of vasoconstrictor substances. The rapid cooling rate, typically achieving therapeutic temperatures within 2-3 seconds, ensures precise control over the depth and duration of tissue cooling. This precision allows practitioners to target specific tissue layers while minimizing damage to deeper structures.
Controlled Vascular Modulation
The controlled nature of CO₂ cryotherapy enables precise manipulation of vascular responses through careful regulation of temperature, duration, and application techniques. Treatment protocols typically involve 10-15 second applications, allowing sufficient time for vasoconstriction without causing tissue damage. The subsequent warming phase initiates the vasodilatory response, creating the beneficial vascular cycling effect. This controlled approach distinguishes CO₂ cryotherapy from traditional ice applications, which often produce unpredictable cooling patterns and prolonged vasoconstriction. The ability to modulate vascular responses precisely makes CO₂ cryotherapy particularly effective for treating inflammatory conditions, promoting tissue repair, and enhancing athletic recovery while minimizing adverse effects.
The Clinical Benefits of Vascular Cycling in CO₂ Cryotherapy
The therapeutic benefits of CO₂ cryotherapy stem directly from its ability to induce controlled vascular cycling, creating optimal conditions for tissue healing and inflammation resolution. Understanding these clinical applications provides insight into why this therapy has gained widespread acceptance in medical and sports medicine settings.
Inflammation Control
Inflammation represents a complex biological response that, while necessary for healing, can become counterproductive when excessive or prolonged. CO₂ cryotherapy’s vascular cycling mechanism provides an effective means of modulating inflammatory responses to promote optimal healing outcomes.
Vasoconstriction in Early Inflammation
The initial vasoconstrictor response during CO₂ cryotherapy serves multiple anti-inflammatory functions that help control the acute inflammatory response. Reduced blood flow limits the delivery of inflammatory mediators to affected tissues, preventing excessive accumulation of pro-inflammatory cytokines. Local cryotherapy significantly reduced IL-6, IL-1β, VEGF, NF-kB-p65, and PG-E2 synovial levels, demonstrating the therapy’s ability to modulate key inflammatory pathways. Additionally, vasoconstriction reduces vascular permeability, limiting tissue edema and preventing the accumulation of inflammatory exudate that can impede healing. This controlled reduction in inflammatory activity helps prevent the transition from acute to chronic inflammation, which often underlies persistent pain and delayed recovery.
Vasodilation and Healing Phase
The subsequent vasodilatory phase creates optimal conditions for tissue repair and inflammation resolution. Enhanced blood flow delivers increased concentrations of anti-inflammatory mediators, growth factors, and immune cells necessary for effective healing. Exposure to cryotherapy may reduce inflammation by reducing the level of proinflammatory factor IL-1β and increasing the level of anti-inflammatory factor IL-10. The improved circulation also facilitates the removal of inflammatory debris and metabolic waste products that can perpetuate inflammatory responses. This dual-phase approach to inflammation management distinguishes CO₂ cryotherapy from single-mechanism treatments, providing comprehensive inflammatory control that supports both immediate symptom relief and long-term healing.
Accelerated Muscle Recovery
Muscle recovery following intense exercise or injury involves complex physiological processes that can be significantly enhanced through strategic vascular manipulation. CO₂ cryotherapy’s ability to induce controlled vascular cycling creates optimal conditions for muscle repair and regeneration. The initial vasoconstriction reduces muscle metabolic demands while limiting the accumulation of metabolic byproducts that contribute to fatigue and soreness. Cryotherapy with carbon dioxide hydrate enhances immediate recovery of muscle function from neuromuscular fatigue. The subsequent vasodilation delivers increased oxygen and nutrients to muscle tissues while facilitating the removal of lactate, creatine kinase, and other markers of muscle damage. This enhanced circulation also promotes the delivery of satellite cells and growth factors necessary for muscle fiber repair and adaptation.
Joint and Tendon Relief
Joint and tendon pathologies often involve chronic inflammatory processes that respond favorably to the controlled vascular cycling induced by CO₂ cryotherapy. The therapy’s ability to modulate synovial fluid dynamics and periarticular blood flow creates therapeutic benefits for various musculoskeletal conditions. Vasoconstriction reduces intra-articular pressure and limits the inflammatory cascade within synovial tissues. The subsequent vasodilation enhances the delivery of synovial fluid nutrients and facilitates the removal of inflammatory mediators from joint spaces. For tendon pathologies, the vascular cycling effect promotes enhanced blood flow to typically hypovascular tendon tissues, supporting collagen synthesis and repair processes. This improved circulation also helps resolve chronic inflammatory changes that often perpetuate tendon pain and dysfunction.

Studies on CO₂ Cryotherapy and Blood Flow
Research into CO₂ cryotherapy’s effects on vascular function has provided valuable insights into the mechanisms underlying its therapeutic benefits. This growing body of evidence supports the clinical application of CO₂ cryotherapy across various medical and athletic contexts.
Research on Skin Perfusion Post-Treatment
Studies examining skin perfusion following CO₂ cryotherapy have revealed significant improvements in microcirculatory function that persist well beyond the immediate treatment period. Research utilizing laser Doppler flowmetry and near-infrared spectroscopy has demonstrated enhanced skin blood flow for up to 60 minutes post-treatment. These findings suggest that CO₂ cryotherapy creates lasting improvements in microcirculatory function that extend the therapeutic window beyond the immediate cooling effect. The enhanced perfusion appears to result from improved endothelial function, reduced sympathetic vasoconstrictor tone, and increased production of vasodilatory substances. These microcirculatory improvements may contribute to enhanced wound healing, improved tissue oxygenation, and reduced risk of tissue necrosis in compromised tissues.
Documented Increases in Blood Flow and Oxygenation
Multiple studies have documented significant increases in tissue blood flow and oxygenation following CO₂ cryotherapy applications. Research has shown that the reactive hyperemia response can increase tissue perfusion by 200-400% above baseline levels, with peak increases occurring 15-30 minutes post-treatment. Tissue oxygenation measurements using near-infrared spectroscopy have revealed corresponding improvements in tissue oxygen saturation that correlate with enhanced blood flow. These findings support the hypothesis that CO₂ cryotherapy’s primary therapeutic mechanism involves optimization of tissue perfusion and oxygenation. The magnitude and duration of these circulatory improvements appear to be dose-dependent, with optimal responses occurring at treatment durations of 10-15 seconds.
Meta-Analysis and Comparative Studies
Recent meta-analyses examining cryotherapy’s effects on various physiological parameters have provided strong evidence supporting CO₂ cryotherapy’s clinical efficacy. Systematic meta-analysis showed that exposure to cryotherapy may reduce inflammation by reducing proinflammatory factors and increasing anti-inflammatory factors. Comparative studies examining different cryotherapy modalities have consistently shown superior outcomes with CO₂-based systems compared to traditional ice applications or other cooling methods. These studies have demonstrated greater precision in temperature control, more predictable vascular responses, and improved patient comfort with CO₂ systems. The evidence suggests that CO₂ cryotherapy’s unique properties make it particularly effective for applications requiring precise temperature control and predictable vascular responses.
Gaps in Current Research
Despite the growing evidence base supporting CO₂ cryotherapy, several research gaps remain that warrant further investigation. Long-term studies examining the effects of repeated CO₂ cryotherapy treatments on vascular function are limited, particularly regarding potential adaptations in vascular reactivity. Additionally, research comparing CO₂ cryotherapy’s effects across different patient populations, including elderly individuals and those with vascular comorbidities, remains sparse. The optimal treatment parameters for different conditions also require further investigation, as most studies have focused on healthy athletic populations. Future research should also examine the molecular mechanisms underlying CO₂ cryotherapy’s vascular effects, particularly the role of specific vasoactive substances and signaling pathways in mediating therapeutic responses.
Applying CO₂ Cryotherapy Safely and Effectively
The clinical application of CO₂ cryotherapy requires careful consideration of treatment parameters, patient selection, and safety protocols to maximize therapeutic benefits while minimizing risks. This section provides evidence-based guidance for optimal clinical practice.
Best Practices for Maximum Vascular Benefits
Optimal CO₂ cryotherapy application requires adherence to specific treatment protocols that maximize vascular cycling benefits while ensuring patient safety. Treatment duration should be limited to 10-15 seconds per application site to achieve therapeutic cooling without causing tissue damage. The application distance should be maintained at 10-15 centimeters to ensure appropriate cooling while preventing frostbite injury. Multiple treatment sites can be addressed during a single session, with 30-60 second intervals between applications to allow for tissue rewarming. Treatment frequency typically ranges from daily applications for acute conditions to 2-3 times weekly for chronic conditions. Patient positioning should optimize access to treatment areas while ensuring comfort and stability. Pre-treatment assessment should include evaluation of skin integrity, sensation, and circulation to identify potential contraindications or areas requiring modified techniques.
Who Should Avoid It
Several conditions and circumstances represent contraindications to CO₂ cryotherapy that require careful consideration during patient screening. Absolute contraindications include severe peripheral vascular disease, Raynaud’s phenomenon, cold urticaria, and areas of compromised sensation or circulation. Patients with severe cardiac conditions, including recent myocardial infarction or unstable angina, should avoid treatment due to potential cardiovascular responses to cold exposure. Open wounds, infected areas, and malignant lesions represent local contraindications that require treatment modification or avoidance. Pregnancy, particularly during the first trimester, is generally considered a relative contraindication pending further research. Patients taking medications that affect vascular function, including certain antihypertensive agents and vasodilators, may require modified treatment protocols. Age-related considerations include careful monitoring of elderly patients and those with multiple comorbidities who may have altered vascular responses to cold exposure.
Summary: Why the Vascular Rollercoaster Works
The effectiveness of CO₂ cryotherapy lies in its ability to harness the body’s natural vascular cycling for healing. The “vascular rollercoaster” effect—controlled cold exposure causing vasoconstriction followed by vasodilation—optimizes tissue blood flow, controls inflammation, and promotes recovery. Vasoconstriction reduces inflammation and protects tissues, while vasodilation restores nutrient delivery and waste removal for tissue repair. This biphasic response sets CO₂ cryotherapy apart by offering both immediate symptom relief and long-term healing benefits. The precise control of CO₂ systems allows tailored treatments that minimize risks from overcooling. Growing research supports its clinical efficacy, showing improvements in inflammation, blood flow, and patient outcomes. CO₂ cryotherapy is becoming an important tool in rehabilitation, sports medicine, and pain management. As vascular physiology knowledge advances, this therapy’s applications will likely expand, providing new hope for patients facing complex inflammatory and recovery challenges.
FAQs
The “vascular rollercoaster” describes the body’s natural cycle of blood vessel constriction (vasoconstriction) followed by dilation (vasodilation) triggered by cold exposure. CO₂ cryotherapy uses this cycle to reduce inflammation and boost healing by controlling blood flow in targeted areas.
Unlike ice packs, CO₂ cryotherapy rapidly cools the skin without overfreezing tissues, creating a precise, controlled vascular response that enhances both immediate pain relief and long-term tissue repair.
Vasoconstriction minimizes swelling and inflammation initially, while vasodilation boosts oxygen and nutrient delivery later—together accelerating tissue healing more effectively than continuous cold or heat alone.
Yes! The controlled vascular cycling can enhance microcirculation even in chronic inflammation or degenerative conditions, promoting gradual tissue regeneration and pain relief over time.
Overexposure can blunt the beneficial rebound vasodilation, so treatment time and intensity must be carefully managed to maintain the therapeutic “rollercoaster” effect and avoid tissue stress.
Patients often feel an initial cooling sting (vasoconstriction) followed by a warming or tingling sensation as blood flow returns (vasodilation)—these are signs the therapy is working as intended.



