소개
Knee pain is one of the most common musculoskeletal complaints among older adults, affecting mobility, independence, and overall quality of life. Age-related structural changes, chronic inflammation, and long-term joint stress contribute to a high prevalence of knee discomfort, particularly among individuals over 60. While medications and surgical interventions can offer temporary relief, they may carry risks or be unsuitable for certain populations. Non-invasive, localized, and drug-free approaches have gained attention for their potential to manage pain safely and support functional mobility. Among these options, CO₂ cryotherapy, a form of targeted cold therapy, has emerged as a promising modality that can reduce inflammation, modulate pain signaling, and enhance recovery in elderly patients with chronic knee pain.
1. Why Knee Pain Is Common in the Elderly
Understanding why knee pain becomes increasingly prevalent with age helps clarify why targeted, non-drug interventions are valuable.
1.1 Anatomy and Function of the Knee Joint
The knee is a complex hinge joint connecting the femur, tibia, and patella, supported by ligaments, tendons, and cartilage. It facilitates weight-bearing, shock absorption, and locomotion, making it essential for activities such as walking, climbing, and standing. Articular cartilage provides smooth movement and minimizes friction between bones, while synovial fluid nourishes cartilage and maintains joint lubrication. With aging, cartilage loses elasticity, ligaments may stiffen, and surrounding muscles weaken, reducing joint stability. These physiological changes can increase susceptibility to injury, chronic inflammation, and discomfort, highlighting the importance of interventions that support joint function without systemic medication.
1.2 Age-Related Degenerative Changes
Over time, the knee undergoes structural and biochemical changes. Articular cartilage may gradually thin and develop microfissures, diminishing its cushioning ability. Synovial fluid production decreases, reducing lubrication and joint nutrition. Ligament elasticity declines, contributing to instability, while periarticular muscles often experience atrophy, further compromising support. Osteophyte formation or bone spur development may occur as the body attempts to stabilize the joint, sometimes exacerbating pain. These degenerative processes collectively contribute to stiffness, reduced mobility, and chronic discomfort, making older adults particularly vulnerable to knee pain even during low-impact activities.
1.3 Common Contributing Factors
Several factors accelerate the onset or severity of knee pain in elderly populations. Osteoarthritis, the leading cause, results from cartilage degradation and chronic low-grade inflammation. Long-term mechanical stress from occupations, sports, or repetitive movements can exacerbate wear and tear. Previous injuries or surgical interventions, such as meniscal tears or ligament repairs, may predispose joints to chronic pain. Additionally, excessive body weight increases mechanical load on knee structures, accelerating cartilage breakdown and promoting inflammation. Understanding these contributing factors is essential for designing interventions that not only relieve symptoms but also target underlying biomechanical and inflammatory processes.
2. Common Symptoms of Knee Pain in Older Adults
Recognizing the typical symptoms helps patients and caregivers identify knee issues early and select appropriate interventions.
2.1 Types of Pain and Sensory Manifestations
Knee pain can manifest in various ways, including aching, sharp, or burning sensations. Activity-related pain is common during walking, climbing stairs, or prolonged standing. Many older adults experience stiffness after prolonged rest or upon waking, commonly referred to as morning stiffness. Pain intensity may fluctuate with weather changes or activity level, and swelling or tenderness may accompany exacerbations. Chronic knee discomfort can be aggravated by microtrauma, inflammatory processes, or joint instability, creating a cycle of pain that reduces functional capacity. Accurate symptom characterization is crucial for tailoring treatment plans, including non-drug modalities such as localized cryotherapy.
2.2 Functional Limitations
Knee pain often leads to functional restrictions, including reduced walking distance, difficulty standing from seated positions, and impaired balance. Activities requiring bending or squatting, such as climbing stairs, may become challenging. These limitations can lead to compensatory movement patterns, increasing the risk of falls and placing additional stress on adjacent joints. Functional decline not only affects mobility but also interferes with social engagement, exercise participation, and independence. Non-invasive interventions that alleviate pain and support joint mechanics can mitigate these functional impairments, enhancing older adults’ ability to maintain active lifestyles.
2.3 Impact on Quality of Life
Chronic knee discomfort significantly impacts emotional well-being, sleep quality, and daily activities. Persistent pain can cause frustration, anxiety, or depressive symptoms, further exacerbating the perception of discomfort. Sleep disturbances, common among individuals with knee pain, reduce restorative rest and can amplify sensitivity to pain. Limitations in mobility may restrict social interactions, hobbies, and self-care routines. Addressing both the physiological and psychological aspects of knee pain is critical, making non-drug interventions such as CO₂ cryotherapy a valuable complement to conventional management strategies aimed at improving overall quality of life.
3. Limitations of Conventional Knee Pain Management
Before exploring non-invasive approaches, it is important to understand why traditional treatments may be insufficient for many elderly patients.
3.1 Common Pharmacological Treatments
Medications frequently prescribed for knee pain include nonsteroidal anti-inflammatory drugs (NSAIDs), acetaminophen, or topical analgesics. These drugs aim to reduce pain and inflammation but often provide only partial relief. Long-term NSAID use carries risks such as gastrointestinal irritation, cardiovascular effects, or kidney dysfunction, particularly in older adults with comorbidities. Opioids may be considered for severe pain but are generally avoided due to dependency risk and side effects. Although effective for acute flare-ups, pharmacological strategies alone may not adequately address chronic functional limitations or tissue-level recovery needs.
3.2 Surgical Interventions Are Not Always Suitable
Surgical procedures, including total or partial knee arthroplasty, can improve mobility in severe cases. However, surgery carries inherent risks such as infection, delayed healing, anesthesia complications, and prolonged rehabilitation. Older adults may have comorbidities that increase surgical risk or limit postoperative recovery potential. Additionally, surgery does not prevent future degenerative changes in adjacent joints. As a result, many elderly patients seek non-invasive strategies that can reduce pain, support joint function, and improve quality of life without requiring major interventions.
3.3 Growing Interest in Non-Drug Approaches
Given the limitations of medications and surgery, there is increased interest in non-pharmacological, non-invasive treatments. These approaches prioritize safety, minimize systemic exposure, and can be integrated into long-term pain management plans. Modalities such as physical therapy, exercise, low-level laser therapy, and CO₂ cryotherapy provide complementary strategies that address underlying inflammation, neuromuscular dysfunction, and localized tissue health, offering a more sustainable approach to chronic knee pain management.
4. Importance of Non-Drug Knee Pain Management
Non-drug interventions are particularly valuable in older populations due to safety, feasibility, and the potential for long-term symptom control.
4.1 Advantages of Non-Invasive Therapies
Non-invasive therapies carry minimal procedural risk, can be administered repeatedly, and are generally well-tolerated by elderly patients. They provide targeted relief without systemic medication exposure, which is particularly important for individuals taking multiple prescriptions. Techniques such as localized cold therapy, physical rehabilitation, and low-level laser therapy focus on supporting tissue healing, reducing inflammation, and improving joint function, often with measurable functional benefits. This approach allows patients to maintain independence and mobility while minimizing the adverse effects associated with pharmacological interventions.
4.2 Significance of Localized Treatment
Targeted interventions can concentrate therapeutic effects directly on the affected joint, reducing inflammation and pain at the source. Localized treatment minimizes systemic stress and supports tissue-specific recovery, which is critical for maintaining functional mobility. For knee pain, this can include modalities such as CO₂ cryotherapy, which delivers controlled cold energy to the joint, or photobiomodulation to stimulate cellular repair. Localized strategies complement broader exercise or rehabilitation programs, enhancing overall effectiveness and providing safe, patient-centered options for chronic pain management.
5. CO₂ 냉동 요법 for Elderly Knee Pain
Among non-drug approaches, CO₂ cryotherapy has emerged as a scientifically supported option with several mechanisms relevant to joint pain relief.
5.1 What Is CO₂ Cryotherapy?
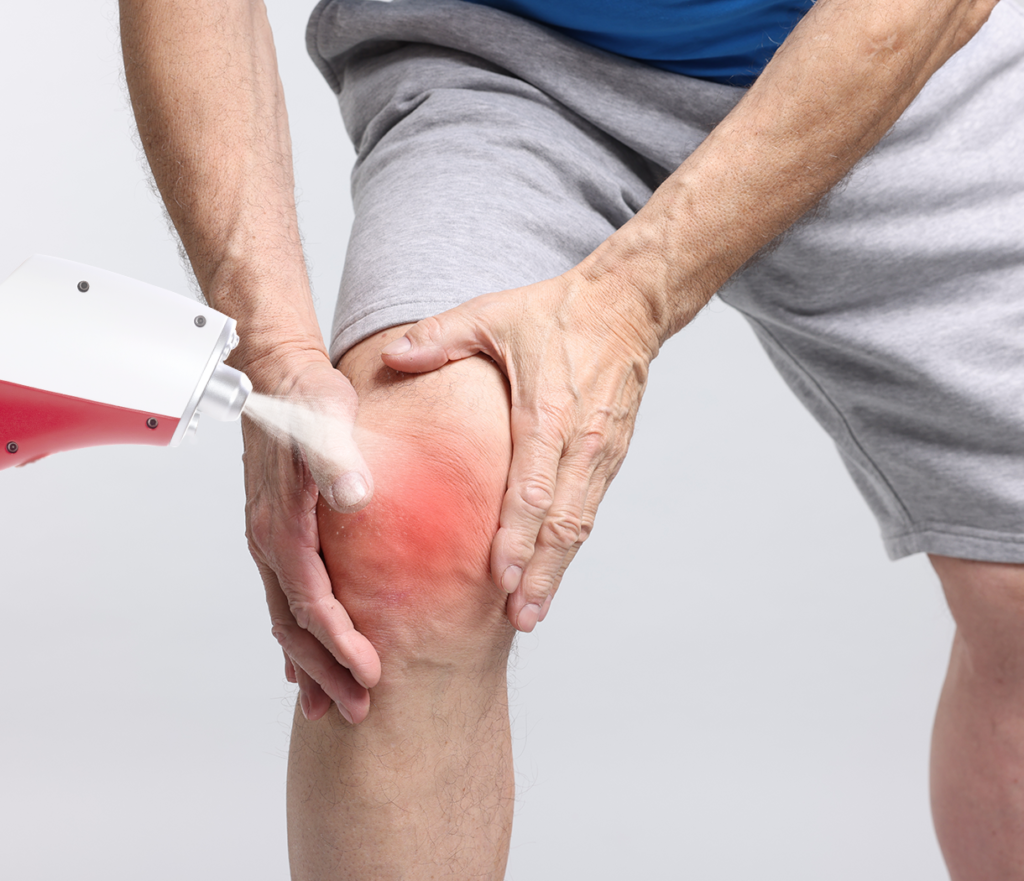
CO₂ cryotherapy involves the application of carbon dioxide in a controlled cold form, typically at temperatures around −78°C, to a localized area. Unlike traditional ice packs, CO₂ cold therapy provides precise, uniform cooling without excessive tissue damage. This modality is non-invasive, short-duration, and designed to minimize discomfort. Its mechanism leverages vasoconstriction followed by reactive hyperemia to modulate inflammatory mediators and promote tissue recovery. CO₂ cryotherapy has been applied in sports medicine, rehabilitation, and chronic pain management, offering a safe option for elderly patients seeking non-drug relief.
5.2 How CO₂ Cryotherapy Works on Knee Joints
Targeted CO₂ cold therapy reduces local inflammation by suppressing pro-inflammatory cytokines and decreasing edema in periarticular tissues. The cold stimulus also modulates nociceptive signaling, reducing pain perception through peripheral and central mechanisms. Reactive hyperemia following treatment enhances oxygen and nutrient delivery to cartilage and surrounding tissues, supporting cellular metabolism and recovery. Additionally, localized cooling may improve joint function by reducing muscle spasm and stiffness. This combination of anti-inflammatory, analgesic, and tissue-supportive effects makes CO₂ cryotherapy particularly suitable for chronic knee pain in elderly individuals.
5.3 Potential Benefits for Older Adults
For seniors with knee discomfort, CO₂ cryotherapy offers several advantages. It is non-drug, avoiding interactions with other medications or systemic side effects. Treatments are brief, painless, and can be administered in a clinical or rehabilitation setting. Regular application may reduce joint pain, enhance mobility, and support participation in daily activities or exercise programs. While not a cure, CO₂ cryotherapy serves as an effective adjunctive therapy, allowing elderly patients to maintain independence, reduce discomfort, and potentially delay the need for invasive interventions.
6. Safety and Practical Considerations
Proper administration and patient selection are critical for safe and effective CO₂ cryotherapy use.
6.1 Safety Considerations for Elderly Patients
CO₂ cryotherapy is generally well-tolerated, even in older adults. Mild transient tingling or warmth at the application site is common but typically resolves quickly. Patients with certain medical conditions, such as severe peripheral vascular disease, neuropathy, or cold intolerance, should be evaluated prior to treatment. Supervision by trained professionals ensures safe temperature control and appropriate exposure duration, reducing the risk of adverse reactions. Overall, CO₂ cryotherapy is a low-risk, non-invasive option for elderly patients seeking localized knee pain relief.
6.2 Treatment Frequency and Professional Guidance
Optimal therapeutic effects often require multiple sessions, with frequency and duration individualized based on pain severity, functional limitations, and overall health status. Professional assessment helps determine the correct treatment parameters, including exposure time, cold intensity, and joint positioning. Integrating CO₂ cryotherapy into a comprehensive care plan, including exercise, stretching, and functional rehabilitation, maximizes benefits. Regular monitoring ensures safety and effectiveness while allowing adjustments based on patient response and tolerance.
자주 묻는 질문
Is knee pain in older adults always due to osteoarthritis?
No, knee pain can result from various factors including ligament injuries, meniscal tears, chronic inflammation, or overuse. Osteoarthritis is the most common cause but not the sole factor.
Can non-drug treatments really help?
Yes, therapies such as CO₂ cryotherapy, physical therapy, and low-level laser therapy can reduce pain, improve joint function, and support mobility, especially when combined with exercise and lifestyle modifications.
Is CO₂ cryotherapy safe for long-term use?
When administered under professional guidance, CO₂ cryotherapy is generally safe for repeated sessions, with minimal risk of adverse effects.
Can cold therapy be combined with other treatments?
Yes, CO₂ cryotherapy can complement medications, physical therapy, or exercise programs to provide a comprehensive approach to pain management.
결론
Elderly knee pain is a multifactorial condition resulting from degenerative changes, chronic inflammation, and mechanical stress. While medications and surgery have their place, non-invasive, localized approaches such as CO₂ cryotherapy provide a safe, effective adjunct for managing pain and improving function. By reducing inflammation, modulating pain signaling, and enhancing joint tissue recovery, CO₂ cryotherapy supports elderly individuals in maintaining mobility and quality of life. When integrated into a comprehensive care plan under professional guidance, this therapy offers a viable, non-drug option for sustainable knee pain management.
참조
National Institute on Aging – Joint Pain and Osteoarthritis
https://www.nia.nih.gov/health/joint-pain-osteoarthritis
Mayo Clinic – Knee Pain in Older Adults: Causes and Treatments
https://www.mayoclinic.org/diseases-conditions/osteoarthritis/expert-answers/knee-pain/faq-20058400
Local Cryotherapy – The Science Behind CO₂ Cryotherapy in Pain Management and Inflammation Reduction
Hamblin, M. R. (2017) – Mechanisms and applications of photobiomodulation
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5523874
Smith, B. et al. (2015) – Non-pharmacological management of knee osteoarthritis in older adults


