소개
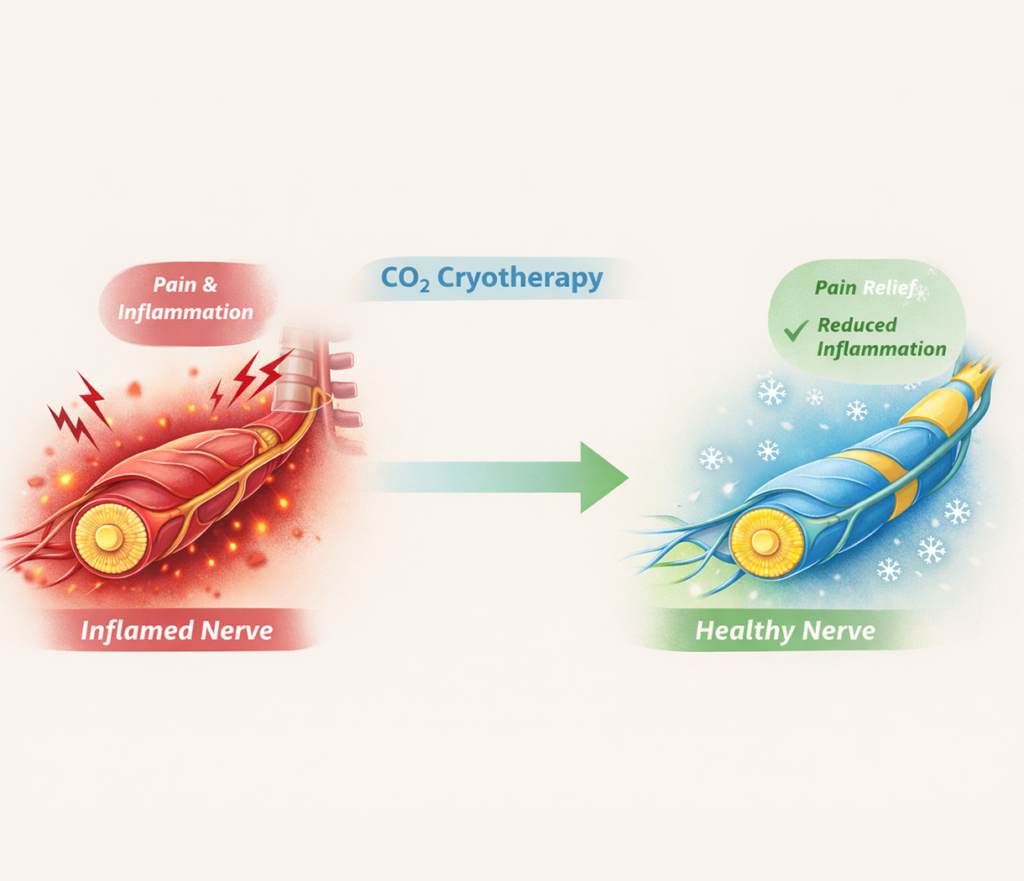
Nerve inflammation, or neuritis, is a common neurological condition that can lead to acute or chronic pain, sensory disturbances, and motor dysfunction. Patients often experience burning sensations, tingling, numbness, and difficulty performing daily activities. Conventional therapies typically include non-steroidal anti-inflammatory drugs (NSAIDs), analgesics, corticosteroids, and physical therapy. While these methods can provide partial relief, they often fall short in addressing the underlying pathophysiology of nerve inflammation and may carry side effects with long-term use. CO₂ cryotherapy (CO₂ cold therapy) has emerged as a safe, non-invasive modality capable of reducing local nerve excitability, modulating inflammatory processes, and promoting tissue repair. By inducing controlled thermal shock, CO₂ cryotherapy triggers neurovascular responses, enhances endogenous pain inhibition, and supports nerve recovery. This article explores the mechanisms, clinical applications, treatment protocols, and evidence-based benefits of CO₂ cryotherapy in managing nerve inflammation and pain.
1. Scientific Background of Nerve Inflammation and Pain
1.1 Types and Symptoms of Neuritis
Neuritis can manifest in various forms, including peripheral neuropathy, central neuritis, and compression-related nerve pain. Symptoms may vary based on nerve type and location but commonly include burning, tingling, numbness, muscle weakness, and functional deficits. Early detection is crucial, as prolonged inflammation may cause irreversible nerve damage. Understanding the specific type of nerve inflammation allows clinicians to tailor therapeutic interventions effectively, combining pharmacological and non-pharmacological strategies such as CO₂ cryotherapy to optimize recovery.
1.2 Conventional Treatments and Limitations
Traditional management of nerve inflammation involves pharmacologic agents like NSAIDs, anticonvulsants (e.g., gabapentin), local anesthetics, and corticosteroids. Physical modalities, including heat, massage, and therapeutic exercises, are frequently employed. However, these approaches may provide incomplete pain relief and often fail to address the molecular mechanisms of chronic nerve inflammation. Long-term medication use carries risks, including gastrointestinal, renal, and hepatic complications. Non-invasive adjunctive therapies, such as CO₂ cryotherapy, offer a complementary approach with minimal side effects, enhancing patient outcomes.
1.3 Pain Mechanisms and Neural Transmission
Pathological pain in nerve inflammation arises from multiple mechanisms, including peripheral sensitization, abnormal nociceptor activation, and inflammatory cytokine release. In affected nerves, inflammatory mediators enhance excitability, leading to amplified pain signals transmitted to the central nervous system. Thermal interventions like CO₂ cryotherapy target these mechanisms by modulating nociceptor activity, reducing inflammation, and improving microcirculation. Understanding these neural pathways is fundamental to appreciating the therapeutic role of cold therapy in pain modulation.
2. Mechanisms of CO₂ Cryotherapy
2.1 Overview of CO₂ Cryotherapy
CO₂ cryotherapy is a non-invasive treatment that delivers high-pressure carbon dioxide gas at temperatures near -78°C to the target area. Unlike conventional ice packs, CO₂ cryotherapy provides precise, deep, and uniform cooling that triggers a controlled thermal shock response in tissues. This intervention reduces local nerve excitability, induces vasoconstriction followed by reactive hyperemia, and stimulates cellular stress pathways. CO₂ 냉동 요법 장치 are designed for clinical use, enabling standardized, reproducible treatment protocols.
2.2 Neural Modulation Mechanisms
Cold exposure from CO₂ cryotherapy inhibits pain signal transmission by suppressing nerve fiber conduction velocity and reducing nociceptor sensitivity. Additionally, cold therapy activates endogenous analgesic pathways, including endorphin release, which attenuates pain perception. Microvascular responses increase oxygen and nutrient delivery to affected nerves while facilitating metabolic waste clearance. These mechanisms collectively diminish hyperalgesia and promote functional recovery, making CO₂ cryotherapy effective for both acute and chronic nerve-related pain.
2.3 Anti-Inflammatory and Tissue Repair Mechanisms
CO₂ cryotherapy also modulates inflammatory pathways by reducing pro-inflammatory cytokine expression, limiting local edema, and mitigating oxidative stress. Thermal shock induced by localized cold exposure stimulates heat shock proteins (HSPs), which play a critical role in cellular repair and protein stabilization. This process supports axonal regeneration and neural tissue recovery. Furthermore, enhanced microcirculation facilitates collagen synthesis and soft tissue remodeling, contributing to structural repair of inflamed nerves.
3. Clinical Applications of CO₂ Cryotherapy in Neuritis
3.1 Peripheral Neuritis
Peripheral neuritis, including carpal tunnel syndrome or post-traumatic neuropathies, benefits from CO₂ cryotherapy through localized pain reduction and inflammation control. Treatment sessions are typically short, ranging from 10 to 15 seconds per affected site, repeated multiple times per week depending on severity. Cryotherapy reduces hypersensitivity, improves local circulation, and enhances nerve function. By complementing pharmacological interventions, CO₂ cold therapy offers a safe and effective method to accelerate recovery and restore functional capacity.
3.2 Compression-Related Nerve Pain
Compression neuropathies, such as lumbar radiculopathy or sciatica, involve mechanical pressure on nerve roots leading to inflammation and pain. CO₂ cryotherapy provides targeted cooling that alleviates nociceptor hyperactivity and reduces perineural edema. The therapy’s rapid analgesic effect allows patients to engage more effectively in physical therapy and exercise programs, which further relieve compression and strengthen supporting musculature. Integrating CO₂ cryotherapy into rehabilitation protocols enhances both pain management and functional outcomes.
3.3 Chronic Pain Syndromes
Patients with chronic pain syndromes, including fibromyalgia and neuropathic pain, often experience persistent discomfort and limited response to conventional treatments. CO₂ cryotherapy modulates central and peripheral pain pathways, providing temporary analgesia and reducing flare-ups of hyperalgesia. Regular, controlled sessions can improve quality of life, decrease reliance on medication, and facilitate participation in daily activities. Safety and tolerability make it suitable for long-term adjunctive therapy in chronic pain management plans.
4. Treatment Protocol and Safety Considerations
4.1 Pre-Treatment Assessment
Before initiating CO₂ cryotherapy, clinicians should evaluate nerve function, skin integrity, and circulatory status. Assessment ensures safety and identifies any contraindications, such as cold hypersensitivity, Raynaud’s phenomenon, or open wounds. Baseline pain and sensory function measurements are recommended to monitor treatment efficacy over time. Proper patient selection is critical to achieving optimal therapeutic outcomes and minimizing adverse reactions.
4.2 Treatment Procedure
During therapy, the CO₂ cryotherapy device is positioned approximately 1–2 cm from the skin surface, and the cold gas is applied to targeted nerve regions. Operators follow a standardized protocol regarding duration, number of passes, and treatment frequency. Typically, sessions last 10–15 seconds per site, with multiple repetitions per week. Controlled movement of the gas nozzle ensures uniform coverage and prevents overexposure. The procedure is generally painless, and patients can resume normal activities immediately afterward.
4.3 Safety and Contraindications
CO₂ cryotherapy is generally well-tolerated, with minimal side effects. Temporary skin redness, numbness, or mild discomfort at the treatment site may occur. Contraindications include severe cold sensitivity, active skin lesions, impaired peripheral circulation, and certain autoimmune disorders. Proper device calibration and adherence to clinical protocols are essential to prevent frostbite or tissue damage. Continuous monitoring during treatment ensures patient safety and treatment efficacy.
자주 묻는 질문
Is CO₂ cryotherapy safe for long-term use?
Yes, when applied according to standard protocols, CO₂ cryotherapy is safe for repeated sessions, with minimal adverse effects.
How quickly does pain relief occur?
Patients may experience immediate analgesic effects, but optimal benefits often require multiple sessions over several weeks.
Can CO₂ cryotherapy replace medications entirely?
It serves as an adjunct therapy. While it may reduce the need for pain medications, complete replacement should only be considered under medical supervision.
How frequently should treatments be administered?
Initial treatment is typically 2–3 times per week, with adjustments based on response and clinical guidance.
Are there any risks or side effects?
Mild, temporary skin redness or numbness may occur. Severe complications are rare when protocols are properly followed.
결론
CO₂ cryotherapy offers a safe, non-invasive, and effective approach for managing nerve inflammation and pain. By modulating nociceptive signaling, reducing inflammation, and promoting tissue repair, it improves patient comfort, functional capacity, and overall quality of life. When integrated with pharmacological treatments, physical rehabilitation, and lifestyle management, CO₂ cryotherapy provides a comprehensive strategy for both acute and chronic neuritis. Ongoing research continues to support its efficacy and safety, highlighting its role as an essential tool in modern pain management protocols.
참조
Local Cryotherapy. The Expanding Role of CO₂ Cryotherapy Devices in Modern Medicine.
Local Cryotherapy. How CO₂ Cryotherapy Triggers the Body’s Natural Regeneration.
Local Cryotherapy. On-the-Go CO₂ Cryotherapy for Multi-Location Success.
https://www.localcryotherapy.com/on-the-go-co%E2%82%82-cryotherapy-for-multi-location-success.html
Local Cryotherapy. CO₂ Cryotherapy in Pain Management and Inflammation Reduction.
Bagnato, G., et al. Cryotherapy in Peripheral Neuropathic Pain: Mechanisms and Clinical Outcomes. Journal of Pain Research, 2021.
Mourot, L., et al. Local Cryotherapy for Pain Management: Physiological Effects and Applications. European Journal of Applied Physiology, 2019.
https://link.springer.com/article/10.1007/s00421-019-04197-3


