소개
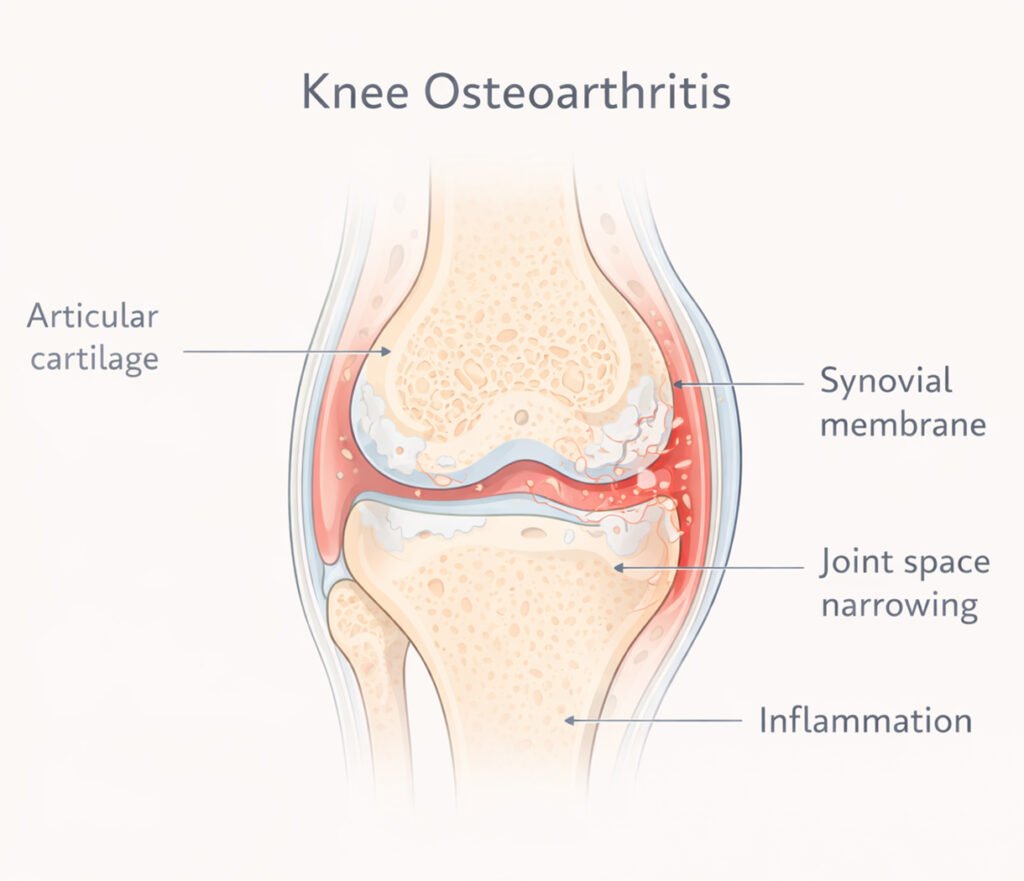
Knee osteoarthritis (KOA) is a degenerative joint disease characterized by the breakdown of cartilage, inflammation of synovial tissues, and changes in subchondral bone structure. Patients typically experience pain, stiffness, swelling, and reduced mobility, which can significantly impact quality of life. Traditional management strategies for KOA include pharmacologic interventions such as non-steroidal anti-inflammatory drugs (NSAIDs), corticosteroid injections, physiotherapy, and in severe cases, surgical options like knee replacement. However, these treatments often provide temporary relief or carry risks of side effects. CO₂ Cryotherapy, an innovative non-invasive approach, has gained attention for its ability to reduce inflammation, improve circulation, and promote joint recovery, making it a promising adjunctive therapy for KOA patients.
1. What is Knee Osteoarthritis (KOA)?
Knee osteoarthritis is a complex, multifactorial disorder that affects millions worldwide. Understanding its pathology and contributing factors is essential to appreciate the rationale behind novel therapies such as CO₂ Cryotherapy.
1.1 Definition and Symptoms
KOA is defined as the progressive degeneration of articular cartilage in the knee joint, often accompanied by subchondral bone remodeling and synovial inflammation. Patients typically present with chronic knee pain, stiffness after periods of inactivity, swelling due to synovial effusion, and decreased range of motion. Pain is often activity-related, worsening with walking, climbing stairs, or prolonged standing. Over time, the mechanical instability may cause altered gait patterns, increasing stress on other joints. Clinically, KOA severity is assessed using imaging modalities such as X-ray, MRI, and scoring systems like the Kellgren-Lawrence grading scale. Early recognition and intervention are critical to prevent progression and maintain functional mobility.
1.2 Risk Factors
Several risk factors contribute to the onset and progression of KOA. Age is a primary determinant, as cartilage loses resilience and regenerative capacity over time. Obesity increases mechanical load on the knee, accelerating cartilage wear and synovial inflammation. Joint injuries, including ligament tears or meniscal damage, predispose individuals to secondary KOA. Genetic factors also influence cartilage structure and susceptibility to degeneration. Furthermore, repetitive high-impact activities or occupations involving prolonged knee flexion can exacerbate cartilage breakdown. Comorbidities such as diabetes, metabolic syndrome, or inflammatory disorders may worsen symptoms by promoting systemic inflammation. Recognizing these risk factors allows targeted intervention strategies and preventive measures.
2. What is CO₂ Cryotherapy?
CO₂ Cryotherapy, or carbon dioxide cryotherapy, is a therapeutic technique that utilizes super-cooled CO₂ gas to induce localized tissue cooling. This method has been shown to modulate inflammatory pathways, improve vascular perfusion, and promote tissue recovery in musculoskeletal conditions.
2.1 Definition of CO₂ Cryotherapy
CO₂ Cryotherapy involves the application of extremely cold carbon dioxide gas to affected tissues, typically at temperatures ranging from -78°C to -90°C. Unlike whole-body cryotherapy, which exposes the entire body to sub-zero air temperatures, localized CO₂ Cryotherapy targets specific joints or areas of inflammation. The cold stimulus triggers vasoconstriction followed by reactive hyperemia, enhancing oxygen delivery and nutrient transport to the affected tissues. Additionally, the therapy induces analgesic effects by reducing nerve conduction velocity and modulating nociceptive signaling. As a non-invasive intervention, CO₂ Cryotherapy avoids systemic complications associated with pharmacologic treatments while providing localized therapeutic benefits.
2.2 How It Works
The therapeutic mechanisms of CO₂ Cryotherapy are multi-faceted. The initial cold application causes vasoconstriction, temporarily reducing local blood flow and limiting inflammatory mediator accumulation. Subsequently, reactive vasodilation enhances microcirculation, facilitating oxygenation and waste clearance. Cryotherapy also modulates cellular responses, reducing the release of pro-inflammatory cytokines such as IL-1β and TNF-α, while promoting anti-inflammatory mediators. Additionally, cold exposure can diminish synovial edema and joint effusion, alleviating pain and stiffness. At the neuronal level, CO₂ Cryotherapy decreases the transmission of pain signals by slowing nerve conduction in sensory fibers. Together, these mechanisms contribute to functional improvement and symptom relief in KOA patients.
3. Mechanism of CO₂ Cryotherapy in KOA
CO₂ 냉동 요법 addresses the key pathophysiological aspects of KOA by targeting inflammation, joint stiffness, and pain. Its effects on cellular and vascular systems create a therapeutic environment conducive to tissue recovery and functional improvement.
3.1 Reducing Inflammation
Inflammation plays a pivotal role in KOA progression, with synovial tissue releasing pro-inflammatory cytokines that degrade cartilage. CO₂ Cryotherapy mitigates these processes by inducing vasoconstriction that limits inflammatory mediator accumulation during treatment. The subsequent vasodilation enhances the removal of metabolic byproducts and inflammatory molecules. Cryotherapy also directly modulates immune cell activity, reducing macrophage infiltration and pro-inflammatory cytokine expression. By decreasing local inflammatory load, CO₂ Cryotherapy alleviates joint swelling, reduces synovial irritation, and slows cartilage degeneration, ultimately improving pain-free range of motion and daily functional capacity for KOA patients.
3.2 Improving Joint Mobility
Joint stiffness in KOA arises from cartilage loss, synovial inflammation, and periarticular tissue fibrosis. CO₂ Cryotherapy improves joint mobility by enhancing microcirculation, which delivers oxygen and nutrients to synovial and periarticular tissues. The cooling stimulus temporarily relaxes muscular and connective tissue tone, allowing for improved joint articulation. Enhanced circulation also supports the removal of lactic acid and metabolic waste from surrounding muscles, further reducing stiffness. Repeated cryotherapy sessions can promote tissue elasticity, reduce adhesions, and facilitate greater functional range of motion, making daily activities such as walking, climbing stairs, and squatting more comfortable for individuals with KOA.
3.3 Pain Relief
Pain in KOA is multifactorial, resulting from mechanical stress, inflammation, and sensitization of nociceptors within the joint. CO₂ Cryotherapy provides analgesia through several mechanisms. The extreme cold decreases nerve conduction velocity in peripheral sensory fibers, reducing the transmission of pain signals to the central nervous system. Additionally, cryotherapy stimulates the release of endogenous opioids and modulates local inflammatory mediators, attenuating pain perception. By targeting both nociceptive and inflammatory pathways, CO₂ Cryotherapy offers immediate symptomatic relief, which can be particularly valuable for patients seeking non-pharmacologic alternatives to NSAIDs or opioids.
4. Clinical Evidence Supporting CO₂ Cryotherapy for KOA
Evidence from clinical studies and mechanistic research supports the efficacy of CO₂ Cryotherapy in managing KOA symptoms. These findings underscore its potential as an adjunct or alternative therapy for patients seeking non-invasive interventions.
4.1 Clinical Trials
Clinical trials have demonstrated that CO₂ Cryotherapy effectively reduces pain, swelling, and stiffness in KOA patients. Studies report significant improvements in Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC) scores and Visual Analogue Scale (VAS) pain ratings following a series of cryotherapy sessions. Patients often experience increased range of motion and improved functional mobility, with benefits observed after as few as four treatment sessions. Importantly, CO₂ Cryotherapy has a favorable safety profile, with minor side effects such as transient erythema or mild skin cooling sensations, making it suitable for long-term management of chronic osteoarthritis.
4.2 Mechanistic Studies
Mechanistic research elucidates the cellular and vascular effects of CO₂ Cryotherapy that underlie clinical improvements. Studies demonstrate reduced expression of inflammatory cytokines, enhanced endothelial nitric oxide production, and improved microvascular perfusion in treated tissues. Cryotherapy has also been shown to decrease synovial edema and facilitate cartilage preservation in experimental models. By simultaneously addressing pain, inflammation, and tissue perfusion, CO₂ Cryotherapy provides a multi-dimensional therapeutic effect that supports both symptom relief and joint health in KOA.
5. CO₂ Cryotherapy Treatment Protocol
Understanding the proper administration of CO₂ Cryotherapy is critical for achieving optimal outcomes in KOA management.
5.1 Treatment Procedure
CO₂ Cryotherapy is delivered using a specialized device that emits super-cooled carbon dioxide gas through a nozzle directed at the knee joint. The patient is positioned comfortably, and the treatment area is exposed while surrounding tissues are protected. Each session typically lasts between 5 and 15 minutes, depending on the protocol and severity of symptoms. The gas is applied in a controlled manner to ensure uniform cooling while avoiding tissue damage. Patients usually experience a cooling sensation followed by slight warmth as reactive circulation occurs. The procedure is painless, non-invasive, and can be integrated with physical therapy or rehabilitation exercises for synergistic effects.
5.2 Frequency and Duration
Recommended treatment frequency varies with symptom severity and therapeutic goals. Early-stage KOA patients may benefit from 2–3 sessions per week over 3–4 weeks, while chronic cases may require ongoing weekly maintenance. Duration of each session is typically 10–15 minutes. Clinical guidelines emphasize consistency in treatment to maximize anti-inflammatory and analgesic effects. CO₂ Cryotherapy can also be combined with exercise programs to enhance joint mobility and muscle support. Long-term follow-up ensures sustained symptom management and allows adjustment of the protocol based on patient response.
6. Benefits of CO₂ Cryotherapy for KOA
CO₂ Cryotherapy offers several advantages over traditional pharmacologic and surgical interventions, making it an attractive option for KOA patients.
6.1 Non-Invasive and Safe
CO₂ Cryotherapy is non-invasive, requiring no injections, incisions, or anesthesia. This minimizes risk and enhances patient acceptance. Unlike systemic NSAIDs, which can cause gastrointestinal or renal side effects, CO₂ Cryotherapy exerts localized therapeutic effects without systemic toxicity. Its safety profile makes it suitable for elderly patients and those with comorbidities who may be at higher risk for complications from conventional treatments.
6.2 Minimal Side Effects
The therapy is generally well-tolerated, with mild transient side effects such as erythema, tingling, or temporary cold sensation. No long-term adverse events have been reported in clinical studies. These characteristics allow repeated treatments without cumulative risk, making it ideal for ongoing management of chronic KOA symptoms.
6.3 Long-Term Effects
Repeated CO₂ Cryotherapy sessions not only provide immediate pain relief but also promote long-term joint health. By reducing inflammation, improving microcirculation, and supporting tissue repair, cryotherapy can slow disease progression and maintain joint function. Patients often report sustained improvements in mobility, reduced reliance on analgesics, and enhanced quality of life, highlighting its value as part of a comprehensive KOA management plan.
7. When to Consider CO₂ Cryotherapy
CO₂ Cryotherapy can be considered at different stages of KOA, from early intervention to chronic symptom management.
7.1 Early-Stage KOA
Patients with mild symptoms, including occasional stiffness and low-grade pain, may benefit from early cryotherapy. The therapy can reduce inflammation, prevent progression, and complement lifestyle modifications such as weight management and physiotherapy.
7.2 Chronic KOA
For patients with long-standing osteoarthritis, CO₂ Cryotherapy provides effective symptom management. Regular sessions can alleviate persistent pain, improve range of motion, and reduce stiffness, supporting better functional outcomes and daily activity engagement.
7.3 Alternative to Medication or Surgery
CO₂ Cryotherapy serves as a non-pharmacologic alternative for patients who wish to minimize NSAID use or avoid surgical intervention. While advanced KOA may still require surgical options, cryotherapy offers a low-risk, cost-effective approach to symptom relief and joint preservation.
자주 묻는 질문
Q1: How long does it take to see results?
Patients may notice improvement after 2–4 sessions, with optimal benefits observed over several weeks of consistent treatment.
Q2: Is CO₂ Cryotherapy safe for all KOA patients?
Generally safe, though patients with cold hypersensitivity, certain cardiovascular conditions, or skin lesions should consult a healthcare provider.
Q3: Can CO₂ Cryotherapy replace surgery entirely?
It is effective for symptom management but does not reverse advanced structural joint damage; surgery may still be necessary for severe cases.
Q4: Are there any side effects?
Side effects are minimal, usually limited to transient skin redness or cold sensation at the treatment site.
결론
CO₂ Cryotherapy is a safe, non-invasive, and effective intervention for Knee Osteoarthritis. By reducing inflammation, improving circulation, and providing analgesia, it enhances joint mobility and functional capacity. As an adjunct or alternative to traditional treatments, CO₂ Cryotherapy offers long-term benefits with minimal side effects, making it an appealing option for patients seeking innovative approaches to managing KOA and improving quality of life.
참조
CO₂ Cryotherapy for Musculoskeletal Pain: Mechanisms and Clinical Applications
https://www.localcryotherapy.com/
Knee Osteoarthritis: Pathophysiology, Clinical Presentation, and Management
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6265784/
Clinical Efficacy of Localized Cryotherapy in Osteoarthritis
https://www.sciencedirect.com/science/article/pii/S1877056820300314


