Introduction: Give Your Knees a Cool Break
Why Your Knees Deserve Attention
Knee pain is a widespread concern, affecting people of all ages and activity levels. The knee is one of the largest and most complex joints in the human body, and it’s prone to wear and tear over time. According to the Centers for Disease Control and Prevention (CDC), 1 in 4 adults in the U.S. report experiencing knee pain at some point in their lives. As the body’s weight-bearing joint, the knee supports every step, jump, and squat, making it especially vulnerable to chronic conditions like osteoarthritis, ligament injuries, and overuse.
Common Causes of Knee Pain
Knee pain can arise from various conditions, each requiring different management strategies. Common causes include:
- Osteoarthritis (OA): Degeneration of cartilage leads to pain, stiffness, and inflammation.
- Patellofemoral Pain Syndrome (PFPS): Pain around the kneecap due to improper alignment or overuse.
- Ligament Injuries: Damage to the anterior cruciate ligament (ACL) or other stabilizing ligaments can result from sports or trauma.
- Tendinitis and Bursitis: Inflammation of tendons or bursae around the knee joint, often caused by repetitive motions.
Cryotherapy 101: Let’s Cool Things Down
What Is Cryotherapy?
Cryotherapy involves using cold temperatures to treat a variety of conditions, from inflammation to pain relief. The therapeutic principle behind cryotherapy is based on the body’s natural response to cold, which triggers vasoconstriction (narrowing of blood vessels). It minimizes swelling and numbs pain through reduced blood flow. Cryotherapy can be applied locally or systemically, depending on the condition being treated.
- Temperature Range: Cryotherapy temperatures typically range from -78°C to -160°C, with the most common forms being ice packs, ice baths, or nitrogen-based cryotherapy chambers.
- Mechanism: Cold exposure leads to decreased metabolic activity in tissues, which reduces the demand for oxygen and nutrients, thereby slowing down inflammatory processes and promoting faster recovery.
Types of Cryotherapy Explained
Whole Body Cryotherapy (WBC): The entire body is exposed to ultra-cold temperatures (usually nitrogen vapor) in a chamber for a short duration (typically 2–3 minutes).
Localized Cryotherapy: This method targets specific areas of the body with precision, offering relief for conditions such as joint pain, muscle soreness, or post-surgical recovery. A localized cryotherapy treatment can focus on a particular joint or muscle, as is the case with CO₂ localized cryotherapy.
Zoom In: What Is CO₂ Localized Cryotherapy?
How Does CO₂ Cryotherapy Work for Knee Pain?
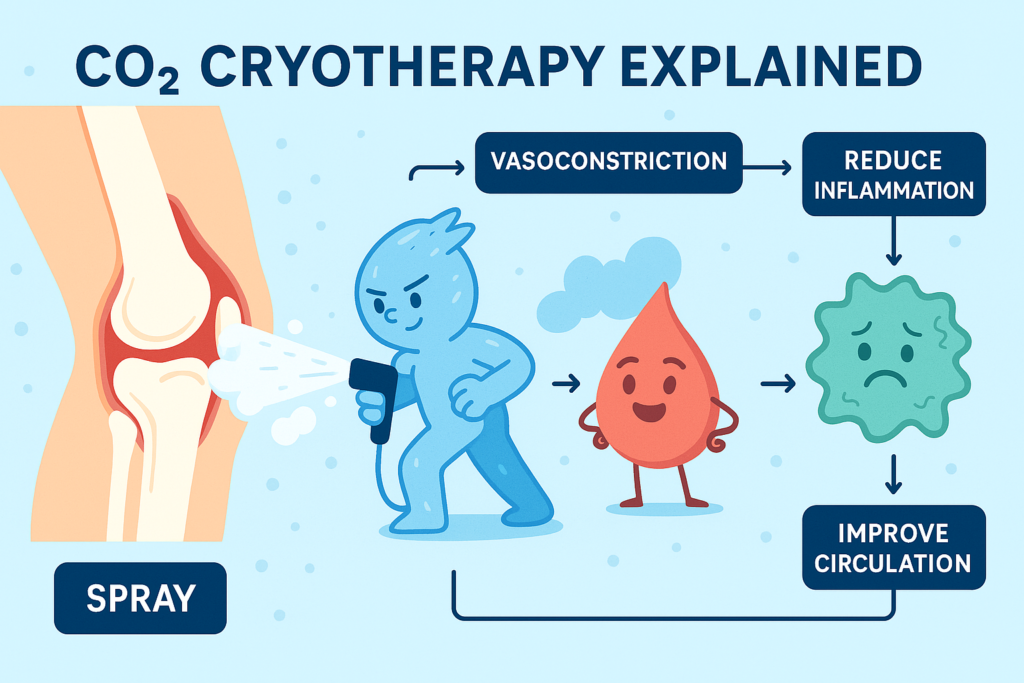
CO₂ localized cryotherapy uses carbon dioxide in its solid form (-78°C) to cool and treat specific areas of the body. The device sprays CO₂ directly onto the targeted area, such as the knee joint, for a brief period of time (typically 10–15 seconds). The primary mechanism is rapid cooling, which causes vasoconstriction and numbs the area, providing immediate pain relief. It can also help reduce inflammation and improve circulation post-treatment, which accelerates healing.
Step-by-step process of CO₂ localized cryotherapy for knee pain:
- Targeted Cooling: A specialized cryotherapy device directs CO₂ onto the knee. The cold penetrates deep into the tissues, targeting the skin, muscles, and joints.
- Vasoconstriction: The cold triggers vasoconstriction, reducing blood flow to the area. This helps limit inflammation and swelling in the joint.
- Rewarming Phase: As the CO₂ dissipates, blood vessels dilate, allowing fresh blood to flow into the area, speeding up recovery and reducing muscle stiffness.
Why CO₂ Over Nitrogen?
While nitrogen-based cryotherapy is commonly used in whole-body cryo chambers, CO₂ cryotherapy is a preferred method for localized treatments. Here are some advantages:
- Temperature Control: CO₂’s temperature of -78°C is ideal for targeting specific areas, offering a precise cooling effect that is effective but less intense than liquid nitrogen cryotherapy, which can be too cold for localized applications.
- Treatment Duration: CO₂ treatments are typically short (10–15 seconds), making them convenient and comfortable for patients. Nitrogen-based systems, especially in whole-body chambers, require longer exposure times.
- Minimal Side Effects: CO₂ localized cryotherapy is less likely to cause adverse effects like skin burns compared to nitrogen treatments, which may cause frostbite if not properly managed.
- Cost-Effective: CO₂ is widely available and often less expensive than nitrogen, making CO₂-based cryotherapy a more accessible option.
Targeting Knee Pain with CO₂ Cryo
Precision Application to Pain Zones
CO₂ localized cryotherapy offers an exceptional level of precision when treating knee pain. Utilizing a high-velocity jet of carbon dioxide gas at –78°C, the system delivers focused cold exposure to specific anatomical zones such as the patellofemoral joint, medial and lateral collateral ligaments, or post-surgical entry points. The device enables therapists to selectively cool inflamed or painful tissues without affecting surrounding healthy areas. This localized approach enhances therapeutic accuracy, promotes faster pain relief, and reduces the likelihood of overcooling or cold-induced tissue damage, which can sometimes occur with whole-body cryotherapy. This makes CO₂ cryotherapy particularly valuable in musculoskeletal conditions where pinpoint control is essential.
Mechanisms of Pain and Swelling Reduction
The therapeutic efficacy of CO₂ cryotherapy lies in its ability to rapidly induce vasoconstriction and modulate pain pathways. When applied to the knee, the extreme cold causes immediate constriction of peripheral blood vessels, thereby reducing local blood flow and minimizing inflammatory exudate formation. This process curbs edema and suppresses the release of pro-inflammatory cytokines such as interleukin-6 (IL-6) and tumor necrosis factor-alpha (TNF-α). Concurrently, the cold stimulus activates the gate control mechanism of pain, disrupting nociceptive transmission via A-delta and C-fibers. Additionally, cold exposure reduces neurogenic inflammation by downregulating the release of neuropeptides like substance P and CGRP. Together, these mechanisms lead to prompt analgesia and support tissue recovery, making CO₂ cryotherapy a powerful non-pharmacologic tool for managing knee joint pathology.
Integration with Physical Therapy
Pre- and post-therapy cryo boosts mobility and recovery during rehab. Pre-therapy application helps reduce pain and stiffness, thereby enabling patients to engage more effectively in stretching, strengthening, and mobilization exercises. Improved comfort and joint flexibility following cryotherapy promote greater range of motion and motor control during active rehabilitation. Post-therapy, cryotherapy supports the recovery of microtrauma induced by exercise and mitigates delayed-onset muscle soreness (DOMS), a common barrier to consistent rehabilitation. Studies suggest that patients undergoing cryo-assisted physiotherapy report improved functional performance and reduced dependency on NSAIDs. By complementing the biomechanical goals of therapy, CO₂ cryotherapy facilitates both short-term symptom control and long-term joint preservation.
Benefits of CO₂ Cryotherapy for Knee Conditions
This therapy is especially beneficial for trauma-related or post-operative knee conditions. One of the most notable advantages is the speed of analgesic effect—patients often experience pain relief within 10 to 15 seconds of application, making it ideal for acute flares or pre-therapy preparation. Unlike oral analgesics or corticosteroid injections, CO₂ cryo avoids systemic side effects and is safe for repeated use. The cold-induced vasoconstriction and neuromodulation not only reduce pain but also limit joint swelling, helping preserve functional movement. Additionally, the therapy’s short duration and non-invasive nature enhance patient compliance. In a clinical setting, CO₂ cryotherapy can be used alongside conventional treatments or as a standalone modality. It is also ideal for on-the-go application in sports settings or mobile clinics, providing both flexibility and efficiency for clinicians and patients alike.
Ideal Candidates for Targeted CO₂ Cryotherapy
Athletes and Active Individuals
CO₂ cryotherapy is particularly well-suited for athletes and physically active individuals who often face overuse injuries or acute joint stress. Whether recovering from ligament strains, tendinitis, or direct trauma, these patients benefit from the immediate cooling and pain relief that CO₂ offers. The rapid application time means athletes can incorporate cryo sessions between training or even courtside, helping to accelerate recovery, reduce inflammation, and restore performance with minimal downtime. It is frequently used as a post-competition tool to alleviate joint stiffness and reduce soft tissue microtrauma.
Older Adults with Chronic Knee Pain
For older adults living with chronic knee pain, especially due to osteoarthritis, CO₂ cryotherapy provides a welcome alternative to long-term drug use. This demographic often experiences joint degradation, cartilage thinning, and chronic inflammation that limit mobility and quality of life. It’s a drug-free option that helps manage flare-ups safely. In many cases, it serves as a bridge to increase participation in low-impact exercises essential for managing joint health.
Post-Operative or Rehab Patients
Patients recovering from procedures such as arthroscopic debridement, ACL reconstruction, or total knee arthroplasty are excellent candidates for localized CO₂ cryotherapy. In the immediate postoperative phase, cryotherapy aids in reducing swelling, controlling pain, and promoting healing at the incision sites. As patients progress into physical rehabilitation, CO₂ therapy can be used to prepare the joint for mobilization by reducing discomfort and increasing flexibility. Its speed and safety make it ideal post-op.
CO₂ Cryotherapy in Physiotherapy: A Smart Add-On
Seamless Integration into Treatment Plans
CO₂ cryotherapy devices are compact, portable, and easy to operate, allowing for seamless incorporation into standard physiotherapy workflows. Because each treatment requires only 10 to 15 seconds per zone, therapists can apply it before or after manual therapy, therapeutic exercises, or neuromuscular reeducation without disrupting the session timeline. The ability to target precise regions means the therapy can be customized based on the patient’s current clinical presentation, such as inflamed bursa, strained ligaments, or surgical scar tissue. This level of integration enhances the overall value and appeal of the physiotherapy session.
Patient-Centered Experience and Compliance
Patients consistently report high satisfaction with CO₂ cryotherapy due to its non-invasive, quick, and tolerable nature. Unlike whole-body cryotherapy, which may induce systemic discomfort or claustrophobia, localized CO₂ treatment is perceived as refreshing and highly tolerable. The immediate pain relief and noticeable reduction in swelling foster a sense of therapeutic success, encouraging patients to adhere to their prescribed rehab plans. Additionally, the absence of direct skin contact with freezing liquids (as seen with ice packs) lowers the risk of frostbite, increasing both safety and comfort.
Economic and Clinical Advantages for Clinics
From a clinical operations standpoint, CO₂ cryotherapy offers strong return-on-investment potential. The cost of CO₂ cartridges is significantly lower than liquid nitrogen, and the devices require minimal maintenance. Because treatments are brief and effective, clinics can accommodate more patients or offer cryotherapy as a premium adjunct service. Furthermore, patients experiencing accelerated recovery and reduced pain are more likely to refer others and maintain long-term relationships with the clinic. When compared to the costs of advanced pharmacotherapy or extended recovery times, CO₂ cryotherapy stands out as a cost-effective, outcome-enhancing solution.
References
Cryotherapy and inflammation: An update on mechanisms and clinical applications:
https://pmc.ncbi.nlm.nih.gov/articles/PMC4698758
Orthopaedic Application of Cryotherapy:
https://www.tigerortho.com/pdfs/research/orthopaedic-application-of-cryotherapy-2021.pdf
Does cryotherapy improve outcomes with soft tissue injury?



