Introduction: Helping Young Pitchers Stay in the Game
Youth baseball has evolved from a recreational pastime into a highly competitive arena where young athletes face unprecedented physical demands. The pitching motion, among the most biomechanically complex athletic movements, generates tremendous forces through developing joints and growth plates. As pitch counts escalate and year-round competition becomes normalized, overuse injuries in young pitchers have reached epidemic proportions. This alarming trend threatens not only immediate athletic participation but also long-term musculoskeletal health and future baseball careers.
The Physical Demands of Youth Baseball Pitching
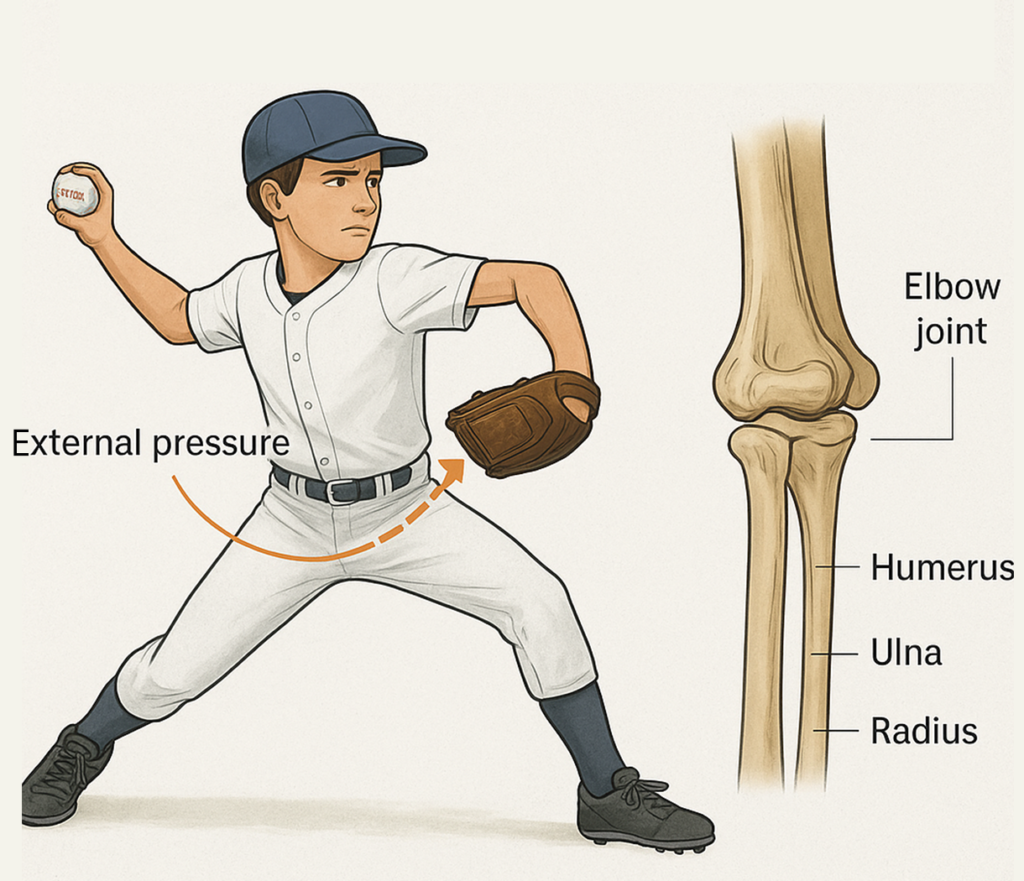
The pitching motion subjects the adolescent elbow to extraordinary biomechanical stress during a critical developmental window. During the late cocking and acceleration phases, valgus forces approaching 64 Newton-meters act upon the medial elbow structures, creating tensile stress on the medial epicondyle where flexor-pronator muscles originate. This attachment site remains vulnerable in youth pitchers because the growth plate (apophysis) here represents a zone of cartilaginous tissue weaker than surrounding bone or tendon. Each pitch generates this repetitive traction force, with professional-level pitchers experiencing loads exceeding body weight by substantial margins. Young throwers attempting to emulate these mechanics with immature skeletal systems accumulate microtrauma that overwhelms healing capacity, particularly when inadequate rest periods prevent tissue recovery between throwing sessions.
Overuse Injuries in Young Throwers —Spotlight on Little League Elbow
Medial epicondyle apophysitis, commonly called Little League elbow, represents the most prevalent injury affecting young baseball pitchers, typically between ages 9 and 14. This overuse condition develops from repetitive traction forces pulling on the medial epicondyle growth plate, causing inflammation, microavulsion, and potential growth disturbance. The injury spectrum ranges from mild apophysitis with localized pain to complete growth plate separation requiring surgical intervention. Contributing factors include excessive pitch counts, inadequate rest between outings, year-round pitching without seasonal breaks, improper mechanics amplifying elbow stress, and premature introduction of breaking pitches generating increased valgus torque. The injury’s prevalence reflects cultural shifts in youth sports emphasizing early specialization, showcase tournaments, and competitive pressures that prioritize short-term performance over long-term athlete development and health.
Why Parents and Coaches Are Turning to CO₂ Cryotherapy for Safer Recovery
Concerned parents and forward-thinking coaches increasingly turn to CO₂ cryotherapy to support young athletes’ recovery safely and effectively. This non-invasive treatment applies localized extreme cold to reduce inflammation, relieve pain, and accelerate healing, aligning with modern sports medicine’s focus on promoting natural recovery rather than merely masking symptoms. Its portability allows immediate post-activity application, targeting critical therapeutic windows for inflammation control. Being drug-free, CO₂ cryotherapy avoids the risks associated with NSAIDs, such as impacts on growth plates or gastrointestinal health. Brief treatments of just 10–15 seconds, with minimal discomfort, make it more acceptable to young athletes who may resist more involved interventions. By improving compliance with recovery protocols, CO₂ cryotherapy supports faster, safer injury resolution while offering parents and coaches a practical, evidence-based alternative that prioritizes the athlete’s long-term health and performance.
Capire la crioterapia CO₂
Cryotherapy, the therapeutic application of extreme cold, has evolved from simple ice pack applications to sophisticated technologies capable of delivering precise thermal shocks to targeted tissues. CO₂ cryotherapy represents an advanced iteration offering superior cooling efficiency, temperature control, and clinical convenience compared to traditional cold therapy modalities.
What Is CO₂ Cryotherapy
Crioterapia CO₂ delivers pressurized carbon dioxide through specialized applicators to produce intense, localized cooling without direct contact or moisture. As compressed CO₂ rapidly changes from liquid to gas, it absorbs significant thermal energy, generating temperatures as low as –78°C at the treatment site—far colder than ice or cold packs. This controlled thermal shock enables deeper, more consistent tissue cooling while minimizing frostbite risk. Modern devices feature precision targeting, often with red laser guidance, ensuring accurate application to specific anatomical points. Integrated temperature monitoring maintains therapeutic levels and prevents overexposure. Treatments are brief, typically lasting 10–15 seconds, providing effective pain relief, inflammation reduction, and accelerated healing without stressing tissue. The non-invasive, drug-free approach allows safer, highly controlled recovery, making CO₂ cryotherapy a practical option for athletes seeking rapid, effective rehabilitation while avoiding the limitations and risks of traditional cold therapy methods.
The Science Behind It —From Cold Shock to Cellular Regeneration
The therapeutic mechanisms of CO₂ cryotherapy extend beyond simple cooling to encompass complex physiological responses initiated by extreme temperature stress. The immediate thermal shock triggers vasoconstriction—rapid narrowing of blood vessels reducing blood flow to the cooled area. This vascular response minimizes hemorrhage and edema formation in acute injuries while decreasing metabolic rate, reducing secondary hypoxic injury from oxygen supply-demand mismatch. Following treatment cessation, reactive hyperemia occurs where blood vessels dilate beyond baseline, dramatically increasing circulation that delivers oxygen, nutrients, and immune cells while removing metabolic waste products. This flush phenomenon enhances tissue healing. At the cellular level, cold exposure activates heat shock proteins and anti-inflammatory signaling pathways while suppressing pro-inflammatory cytokine production. Nerve conduction velocity decreases with cooling, raising sensory thresholds and reducing pain signal transmission. These multilevel effects create an optimal environment for tissue repair and inflammation resolution.
Key Physiological Benefits: Vasoconstriction, Anti-Inflammation, and Faster Healing
CO₂ cryotherapy produces three primary physiological effects that synergistically promote injury recovery. Vasoconstriction immediately following cold application constricts blood vessels, reducing capillary permeability that causes swelling and limiting hemorrhage in acute injuries. This vascular narrowing decreases tissue metabolic rate by up to 70%, reducing oxygen demand and preventing secondary cell death in oxygen-deprived tissues. The anti-inflammatory effect occurs through multiple pathways: decreased pro-inflammatory mediator release, reduced immune cell migration to injury sites, and modulation of inflammatory enzyme activity. Cold therapy has been found to decrease inflammatory reactions in experimental situations, with research demonstrating reduced markers including interleukin-6 and C-reactive protein. Enhanced healing results from the reactive hyperemia following treatment, where increased circulation delivers healing substrates while removing inflammatory debris. Additionally, cold stimulation may activate cellular stress responses that upregulate repair gene expression, promoting tissue regeneration.
Little League Elbow: Causes, Symptoms, and Long-Term Risks
Understanding Little League elbow’s pathophysiology, clinical presentation, and potential complications provides essential context for appreciating CO₂ cryotherapy’s therapeutic role in managing this common yet serious youth pitching injury.
What Exactly Is Little League Elbow? (Medial Epicondyle Apophysitis Explained)
Little League elbow, formally termed medial epicondyle apophysitis, represents inflammation and traction injury at the growth plate where forearm flexor-pronator muscles attach to the medial epicondyle of the humerus. During childhood and early adolescence, this attachment site remains an apophysis—a secondary ossification center separated from the main bone by cartilaginous growth plate tissue. This cartilage proves mechanically weaker than mature bone or tendon, making it the vulnerable link in the muscle-tendon-bone chain. Repetitive traction forces during throwing create microavulsion at the growth plate interface, separating cartilage cells and disrupting the organized columns where longitudinal bone growth occurs. Inflammation develops as the body attempts to repair this ongoing damage, producing pain, swelling, and functional limitation. The condition exists on a spectrum from mild apophysitis to complete avulsion fracture where the entire medial epicondyle separates from the humerus.
Why Repetitive Pitching Stresses the Growth Plate
Repetitive pitching places intense valgus stress on the medial elbow, where outward bending stretches soft tissues and compresses the lateral joint. During the late cocking and acceleration phases, extreme external rotation and rapid forearm movement generate powerful forces that strain the flexor-pronator muscles and their attachment at the medial epicondyle. In young athletes, the cartilaginous growth plate—still developing and weaker than mature bone—absorbs this stress instead of the tendon-bone interface. Repeated tensile loading during growth spurts, when bones lengthen faster than muscles adapt, heightens vulnerability. Each pitch causes microtrauma that, when accumulated over time, surpasses the body’s ability to repair, leading to inflammation, pain, and structural damage known as Little League elbow.
Warning Signs Every Parent and Coach Should Know
The first sign is medial elbow pain during or after throwing that worsens over time.
Pain may radiate down the forearm or appear laterally from joint compression.
Localized tenderness over the medial epicondyle is almost always present.
Swelling around the elbow may become visible after repeated activity.
Decreased throwing velocity and accuracy often accompany increasing pain.
Elbow stiffness, especially difficulty straightening the arm, may indicate joint effusion.
Clicking or locking sensations can signal cartilage damage or loose bodies.
Long-Term Consequences of Ignoring Early Elbow Pain
Ignoring symptoms can lead to complete growth plate separation requiring surgery.
Chronic inflammation may cause premature growth plate closure and elbow deformity.
Repetitive stress increases the risk of articular cartilage damage and early arthritis.
Ongoing strain may result in ulnar collateral ligament injury requiring reconstruction.
Elbow instability can alter throwing mechanics and overload the shoulder.
Secondary injuries such as rotator cuff or labral tears may develop over time.
Persistent pain and reduced performance can discourage young athletes from continuing.
Severe or repeated injury can cause permanent motion loss or daily functional impairment.
How CO₂ Cryotherapy Supports Recovery from Little League Elbow
CO₂ cryotherapy addresses multiple pathophysiological aspects of Little League elbow through its multifaceted effects on inflammation, pain, circulation, and tissue healing. This makes it a valuable component of comprehensive treatment protocols for this common youth pitching injury.
Fast Inflammation and Pain Reduction Without Medication
CO₂ cryotherapy provides rapid relief of inflammation and pain without drugs. Extreme cold triggers vasoconstriction, limiting inflammatory cell infiltration and reducing capillary leakage that causes swelling around the growth plate. Local cooling decreases pro-inflammatory cytokine production, interrupting the cascade of tissue damage. Pain relief arises from multiple mechanisms: slowing nerve conduction raises sensory thresholds, intense cold stimulation triggers gate control analgesia by blocking pain signals, and reduced inflammatory mediators decrease chemical irritation of nociceptors. Patients often notice significant pain reduction within minutes. This rapid, non-invasive effect is particularly valuable for young athletes who resist longer or more invasive interventions. Being medication-free, CO₂ cryotherapy eliminates concerns about NSAID effects on growth plates and developing systems, providing safe, effective symptomatic relief while promoting adherence to recovery protocols.
Enhancing Circulation and Stimulating Cellular Repair
After initial vasoconstriction, CO₂ cryotherapy induces reactive hyperemia, boosting blood flow above baseline. This enhances delivery of oxygen, glucose, amino acids, and other substrates needed for tissue repair, while removing metabolic waste and inflammatory debris. Improved perfusion supports cellular metabolism essential for collagen synthesis, cartilage regeneration, and bone remodeling in the growth plate. Repeated vasoconstriction-hyperemia cycles act as a vascular exercise, potentially improving microcirculation. Cold exposure may also activate stress response pathways, increasing growth factor and repair protein production. These circulatory and cellular effects complement anti-inflammatory benefits, creating an optimal environment for healing apophysitis. By supporting tissue repair at both the vascular and cellular levels, CO₂ cryotherapy accelerates recovery while maintaining growth plate function, reducing long-term complications, and preparing the injured area for safe gradual return to activity.
Supporting Growth Plate Health and Preventing Further Injury
CO₂ cryotherapy protects vulnerable growth plate tissue by reducing pain and inflammation, encouraging compliance with activity restrictions. Cooling decreases metabolic demand, minimizing secondary cell death in the hypoxic growth plate environment. Post-treatment hyperemia delivers nutrients that support chondrocyte viability and function critical for normal growth plate activity. Pain relief enables safe participation in rehabilitation exercises to maintain conditioning and correct mechanical deficiencies without causing further injury. Serial treatments manage persistent low-grade inflammation even during activity modification. By controlling inflammation, preserving cellular health, and supporting functional rehabilitation, CO₂ cryotherapy reduces the risk of avulsion or premature physeal closure. The combination of symptomatic relief, cellular support, and vascular enhancement provides a comprehensive protective strategy for long-term growth plate integrity.
How Cryotherapy Complements Physical Therapy and Rest
CO₂ cryotherapy enhances standard Little League elbow treatments by complementing rest and physical therapy. Pre-treatment applications reduce baseline pain and inflammation, allowing athletes to perform exercises more comfortably and effectively. Post-therapy cryotherapy manages reactive inflammation from rehabilitation sessions, preventing setbacks. When paired with rest, cryotherapy accelerates inflammation resolution, potentially shortening the no-throw period. Pain relief reduces reliance on oral anti-inflammatories, which can negatively affect bone healing. The modality also supports manual therapy, strengthening, and biomechanical correction programs by controlling post-session inflammation. By combining symptomatic relief, tissue protection from rest, and functional restoration through physical therapy, CO₂ cryotherapy creates a comprehensive, integrative approach that addresses all aspects of recovery and facilitates a safer, faster return to throwing.
Practical Application for Young Pitchers
Effective utilization of CO₂ cryotherapy requires understanding optimal timing, proper technique, and appropriate treatment parameters. Practical guidance ensures maximum therapeutic benefit while maintaining safety in young athletes.
When and How to Use CO₂ Cryotherapy After Games or Practice
Timing is crucial to maximize CO₂ cryotherapy’s anti-inflammatory and pain-relieving effects. Application within 15–30 minutes post-activity targets the acute inflammatory phase when edema and mediator release peak, minimizing tissue damage and speeding recovery. Athletes should receive treatment as soon as symptoms appear, following warm-down routines but before inflammation fully develops. Position the athlete comfortably with the affected elbow exposed. Using pressurized CO₂ at around –78°C, the device is aimed at the medial epicondyle with precision targeting, often guided by a red laser. Each site receives 10–15 seconds of cold exposure, sufficient for therapeutic effect without frostbite risk. For diffuse discomfort, multiple medial elbow points may be treated. Immediate, correctly timed application ensures optimal pain reduction, inflammation control, and faster functional recovery.
Safe Localized Application: Step-by-Step for Elbow Treatment
Effective and safe CO₂ cryotherapy requires proper technique. Begin by inspecting the skin for contraindications like wounds, infections, or previous frostbite. Position the athlete seated or lying with the arm relaxed and supported. Identify the medial epicondyle as the treatment target. Activate the device per manufacturer instructions, ensuring temperature monitoring is functional. Hold the applicator perpendicular to the skin, 1–3 cm away, to prevent direct contact while maintaining effective cooling. Apply for 10–15 seconds in small circular motions for even coverage. Monitor for discomfort; mild stinging or cold is normal, but severe pain stops treatment. Skin may redden or blanch, which resolves quickly. Allow intervals between multiple applications if needed. Following these steps ensures precise, safe, and effective localized therapy.
Recommended Frequency and Recovery Duration
Cryotherapy frequency should match injury severity, healing phase, and individual response. During acute symptoms, daily applications optimize inflammation and pain control; some protocols recommend twice daily for 3–5 days. As recovery progresses, frequency decreases to every other day or post-throwing sessions during rehabilitation. Complete recovery typically requires 4–8 weeks of modified activity. Cryotherapy continues to support tissue healing by managing reactive inflammation from gradual return to throwing. Even after symptoms resolve, periodic post-activity sessions may prevent recurrence. Serial treatments over weeks provide cumulative benefits beyond single sessions. Parents and coaches should log each treatment’s timing, duration, and symptom response to guide progression and communicate with healthcare providers, ensuring consistent, evidence-based recovery management.
Beyond Pain Relief: The Full Benefits
While immediate pain and inflammation reduction represent CO₂ cryotherapy’s most obvious benefits, the technology offers additional advantages that significantly impact young pitchers’ recovery trajectories and overall athletic development.
Faster Recovery and Shorter Downtime Between Games
CO₂ cryotherapy accelerates healing, shortening recovery compared to passive rest. By reducing inflammation and edema, it optimizes tissue repair while enhanced circulation delivers nutrients and removes metabolic waste. Controlled metabolic rates minimize secondary tissue damage, allowing faster symptom resolution and earlier return to pain-free throwing. For young pitchers, this reduced downtime is crucial during structured seasons or roster competitions. Rapid recovery also supports earlier reintroduction of strength and conditioning, preventing detraining during rest. Psychologically, seeing tangible progress maintains motivation and adherence to treatment protocols, reducing frustration associated with prolonged recovery. Overall, CO₂ cryotherapy supports both physical and mental readiness, enabling athletes to return to play safely, efficiently, and with sustained performance, making it a valuable tool for youth sports where time lost to injury can significantly impact development and competitive opportunities.
Improved Performance Through Healthy Tissue Conditioning
CO₂ cryotherapy promotes optimal tissue healing, preserving growth plate structure and mechanical properties, avoiding disorganized scar formation. By eliminating residual inflammation, athletes maintain proper throwing mechanics, preventing compensatory patterns that can impair performance. Modified activities during recovery preserve arm conditioning, preventing detraining. Properly managed recovery enhances physiological tissue quality and builds psychological confidence, helping athletes feel stronger upon return. The process also serves as a learning experience, teaching body awareness, self-care, and sustainable training habits that reduce future injury risk. Holistic recovery supported by cryotherapy not only restores pre-injury performance but can improve long-term athletic outcomes, fostering resilience, proper mechanics, and knowledge that supports ongoing healthy development and career longevity in youth sports.

Reduced Risk of Recurrent or Chronic Injuries
CO₂ cryotherapy reduces re-injury risk and prevents chronic conditions by thoroughly resolving inflammation and restoring growth plate tissue capable of handling normal throwing loads. Pain relief enables early, targeted rehabilitation, correcting biomechanical deficiencies that caused the initial injury. Athletes develop confidence in their body’s resilience and in treatment protocols, improving adherence to preventive strategies such as proper warm-up, pitch counts, and early symptom reporting. Educational aspects of cryotherapy teach young athletes about injury mechanisms, recovery, and self-care. By addressing root causes rather than just symptoms and promoting proper tissue adaptation, CO₂ cryotherapy breaks the cycle of incomplete recovery, minimizing recurrence and establishing a foundation for sustained, healthy athletic participation while supporting both physical and long-term behavioral injury prevention.
Restoring Confidence and Motivation in Young Athletes
Injury can negatively affect young athletes’ confidence, social engagement, and motivation. CO₂ cryotherapy aids psychological recovery through rapid symptom improvement, giving tangible evidence of healing and countering helplessness or anxiety. Active participation in treatment fosters a sense of control, while the professional appearance of the technology enhances perceived legitimacy and treatment confidence. Pain relief allows earlier return to team activities, preventing isolation and maintaining social interaction central to youth sports enjoyment. Observing healing progress and experiencing effective, non-invasive care builds resilience, reduces fear of re-injury, and supports safe, confident performance. For athletes whose identity is closely tied to sport, cryotherapy enables physical recovery while preserving self-concept and motivation during critical developmental periods.
Role of Parents and Coaches in Long-Term Injury Prevention
While CO₂ cryotherapy provides valuable therapeutic intervention, preventing Little League elbow and other youth pitching injuries requires comprehensive approaches where parents and coaches play essential leadership roles. Creating cultures prioritizing long-term athlete health over short-term competitive success proves fundamental.
Monitoring Throw Counts and Enforcing Rest Periods
Pitch count limits are the most evidence-based strategy to prevent overuse injuries in young pitchers. Guidelines such as USA Baseball and MLB Pitch Smart recommend age-based maximums: 50 pitches for ages 7–8, 75 for 9–10, 85 for 11–12, and 95 for 13–14, with mandatory rest days increasing with volume. Coaches must track all pitching, including bullpen sessions, and enforce limits despite competitive pressures, while parents advocate for their child’s health. Annual off-season rest of 2–3 months is critical, and athletes should avoid pitching for multiple teams or year-round specialized training. Breaking pitches should follow age guidelines. Adherence dramatically reduces injury risk. Digital tracking tools help monitor cumulative exposure, preventing gradual overuse. Diligent enforcement of pitch counts, combined with planned rest, forms the foundation for safe youth pitching and long-term arm health.
Teaching Early Pain Awareness and Reporting
Encouraging athletes to report discomfort early is essential for preventing serious injuries. Coaches and parents should communicate that elbow pain is abnormal, not a sign of weakness, and requires evaluation. Athletes must understand continuing through pain risks career-impacting injury. Regular check-ins normalize symptom reporting, and teaching anatomical awareness helps distinguish normal fatigue from concerning pain. Positive reinforcement for disclosure, rather than punishment, encourages honesty. Parents should observe indirect signs such as reduced velocity, altered mechanics, or favoring the arm. Building trust with sports medicine professionals ensures open communication. Establishing this proactive culture transforms injury reporting from a feared admission into responsible health management, enabling early intervention and safer recovery for young athletes.
Integrating CO₂ Cryotherapy into Smart Recovery Routines
Routine integration of CO₂ cryotherapy optimizes preventive and therapeutic benefits. Post-game applications normalize recovery, preventing minor inflammation from escalating. Teams can establish locker room cryotherapy stations, while parents may provide home devices for early treatment. Written protocols detailing timing, duration, and frequency ensure consistency. Athletes with previous injuries or risk factors may benefit from additional preventive sessions. Combining cryotherapy with nutrition, hydration, sleep, and age-appropriate strength training creates a comprehensive recovery program. Documenting treatment sessions, symptom responses, and throwing volumes supports informed decisions on activity progression and intervention intensity. Systematic cryotherapy shifts recovery from reactive treatment to proactive health management, reducing injury risk while enhancing safe performance and long-term arm durability.
Promoting Safe Pitching Habits and Balanced Training Loads
Injury prevention extends beyond pitch counts to mechanics, training load, and overall athletic development. Proper mechanics minimizing valgus stress should be taught early and reinforced, with video analysis identifying flaws. Avoiding year-round single-sport specialization reduces overuse risk, while multi-sport participation promotes overall athleticism. Strength programs should emphasize posterior shoulder, scapular, core stability, and functional total-body movements rather than only velocity. Flexibility training addresses growth-spurt-related tightness that increases injury risk. Monitoring total training volume—including practices, games, showcases, and private coaching—prevents cumulative fatigue. Adequate sleep (8–10 hours) and proper nutrition support recovery and growth. Holistic approaches consider multiple interacting factors, ensuring that young athletes develop safely, maintain performance, and minimize overuse injuries while fostering long-term physical health.
Prove e approfondimenti degli esperti
The clinical application of CO₂ cryotherapy for youth sports injuries builds upon extensive research examining cryotherapy’s mechanisms and efficacy. Expert perspectives from sports medicine professionals provide practical context for evidence-based utilization.
Current Research on Cryotherapy for Sports Injury Recovery
Research supports cryotherapy as an effective tool for sports injury recovery. Studies show that cold application reduces inflammation by decreasing pro-inflammatory cytokines and immune cell infiltration. Cryotherapy alleviates muscle soreness, accelerates perceived recovery, and enables faster return to training after intense exercise or injury. Tissue temperature studies confirm therapeutic cooling depths of 2–4 cm, sufficient for most musculoskeletal injuries. Systematic reviews recognize cryotherapy as effective for acute soft tissue injuries when properly applied. Evidence emphasizes cryotherapy works best as part of comprehensive treatment rather than alone. Ongoing research explores optimal temperature, duration, frequency, and timing to maximize benefits while avoiding negative effects. Current data confirm its safety profile, with minimal adverse events when protocols are followed, supporting its inclusion in evidence-based injury management programs.
Pediatric Sports Medicine Perspectives on CO₂ Cryotherapy
Pediatric sports medicine specialists increasingly incorporate CO₂ cryotherapy into youth athlete care, valuing its effectiveness and safety for developing tissues. It is particularly useful for growth plate injuries where medication options are limited. Non-invasive treatment avoids risks associated with injections or surgery. Rapid symptom relief improves compliance with activity restrictions, enabling athletes to accept necessary throwing cessation. Specialists highlight cryotherapy’s role within multimodal care, combined with rest, physical therapy, biomechanical assessment, and education. Proper technique and parameter selection are critical to ensure safety in young athletes. Many pediatric experts advocate cryotherapy as a first-line intervention before progressing to invasive or pharmacological options. Its integration supports safe, efficient, and evidence-based management of pediatric sports injuries.
Expert Insights from Physical Therapists and Athletic Trainers
Physical therapists and athletic trainers emphasize CO₂ cryotherapy’s practical benefits for youth athletes. Pre-rehabilitation applications reduce pain and muscle guarding, improving therapeutic exercise effectiveness. Trainers value field applicability, enabling immediate post-practice or post-game treatment during critical inflammatory windows. Cryotherapy also provides an educational opportunity, teaching athletes about injury mechanisms, recovery, and self-care, fostering long-term health literacy. Athletes often respond positively to the high-tech appeal of CO₂ devices. Clinicians stress that cryotherapy addresses pain and inflammation but must be combined with biomechanical evaluation, manual therapy, and progressive return-to-sport protocols to prevent recurrence. Experienced practitioners develop individualized algorithms integrating cryotherapy with comprehensive care, optimizing both short- and long-term outcomes for youth athletes.
Conclusion: Smarter Recovery, Stronger Future
Integrating CO₂ cryotherapy into youth baseball injury management advances protection for young pitchers against immediate pain and long-term musculoskeletal damage. This non-invasive, drug-free technology reduces inflammation, relieves pain, enhances circulation, and supports tissue healing within 10–15 seconds, with precision targeting and portability enabling immediate post-activity application. Its rapid, effective treatment improves compliance among young athletes and families. However, cryotherapy is one component of comprehensive care, requiring rest, physical therapy, biomechanical correction, education, and cultural changes emphasizing pitch counts, rest, and balanced training. Parents and coaches play crucial roles in monitoring throwing volumes, enforcing limits, and fostering pain-reporting cultures. Evidence supports cryotherapy’s safety and efficacy when applied appropriately, and ongoing research continues to refine best practices. As accessibility increases, CO₂ cryotherapy is poised to become a standard tool in youth sports, promoting faster recovery, safer participation, and sustainable athletic development.



