Introduction: Rethinking Recovery Through Gait and Muscle Balance
The intersection of cryotherapy and biomechanical rehabilitation marks an exciting advancement in modern physical medicine. As clinicians and athletes pursue more refined recovery tools, CO₂ cryotherapy stands out for its targeted neuromuscular effects that go beyond traditional pain relief. Unlike one-size-fits-all methods, this localized cold therapy directly influences gait mechanics and muscle load distribution by triggering precise changes in muscle activation and proprioceptive feedback. Understanding these effects is essential for physical therapists and sports medicine professionals aiming to enhance both recovery and performance. By impacting the body’s kinetic chain, CO₂ cryotherapy helps correct movement dysfunction at its source. This article explores the underlying science and real-world applications of this emerging technology in both clinical and athletic settings.
Understanding CO₂ Cryotherapy in Physical Medicine
The evolution of cryotherapy from simple ice applications to sophisticated CO₂ delivery systems represents a significant advancement in therapeutic precision. To fully appreciate how this technology influences gait and muscle function, we must first understand its fundamental principles and physiological mechanisms.
What Is CO₂ Cryotherapy?
CO₂ cryotherapy delivers pressurized carbon dioxide at around –78°C to rapidly cool targeted tissues. A fine jet of CO₂ is applied for 10–15 seconds, causing immediate vasoconstriction followed by reactive hyperemia. This physiological cascade goes beyond surface effects, influencing neuromuscular responses and recovery. Unlike traditional ice therapy, which cools broadly and slowly, CO₂ cryotherapy provides fast, localized cooling, reducing the risk of overcooling nearby tissues. This is crucial for treating muscle imbalances, joint dysfunction, or gait abnormalities with precision. Immediate effects include skin temperature drop, altered nerve conduction, and modulation of muscle spindle sensitivity. These changes affect motor control, proprioception, and muscle tone, making CO₂ cryotherapy a tool not just for pain relief but also for influencing movement quality and load distribution during gait.
How CO₂ Cryotherapy Interacts with Musculoskeletal and Neuromuscular Systems
CO₂ cryotherapy affects the musculoskeletal and neuromuscular systems by altering nerve conduction and mechanoreceptor sensitivity. Rapid cooling slows motor and sensory nerve conduction, temporarily modifying muscle activation timing and proprioceptive input. This temperature-induced neuromodulation helps correct compensatory movement patterns, improves agonist-antagonist balance, and enhances joint mobility. Mechanoreceptors like muscle spindles and Golgi tendon organs become less reactive, which reduces excessive tone and allows smoother, more coordinated movement. Additionally, the vascular response—vasoconstriction followed by hyperemia—boosts blood flow and nutrient delivery to target areas. This supports tissue repair and enhances outcomes from follow-up gait retraining or therapeutic exercise. The result is a neuromuscular reset that helps restore more efficient biomechanical function.

Differences from Whole-Body Cryotherapy
Whole-body cryotherapy (WBC) cools the entire body using air at –100°C or colder for 2–4 minutes. While WBC may reduce systemic inflammation, it lacks localized precision. In contrast, CO₂ cryotherapy targets specific muscles or joints, making it ideal for treating gait dysfunction or movement impairments. CO₂ cryotherapy can be applied to isolated regions like the calf or hamstring, addressing specific gait issues without influencing unrelated muscles. The short application time (10–15 seconds) limits tissue stress and allows multiple body parts to be treated in one session. Unlike WBC, which often requires time for systemic effects to emerge, CO₂ produces immediate results. Changes in muscle activation and range of motion can be observed in real-time during gait analysis, making it a practical tool for biofeedback and movement correction during rehab sessions.
The Biomechanics Behind Gait and Muscle Load
Gait represents one of the most complex coordinated movement patterns in human physiology, requiring precise timing and load distribution across multiple muscle groups and joint systems. Understanding the intricate biomechanical principles underlying normal and abnormal gait patterns provides the foundation for appreciating how CO₂ cryotherapy can create meaningful therapeutic changes.
What Is Gait and Why It Matters
Gait refers to the coordinated sequence of movements used for walking or running. It involves precise muscle activation, joint mobility, and ground reaction force (GRF) management throughout the kinetic chain. Each gait cycle includes eight phases—from initial contact to terminal swing—requiring tightly timed muscular control to ensure balance, efficiency, and fall prevention. Any disruption in this sequence can lead to compensatory movement patterns, often resulting in pain, joint overload, or reduced performance. Clinically, gait reflects deeper issues like neuromuscular dysfunction, mobility restrictions, or asymmetries in muscle activation. Modern gait analysis tools—tracking variables like cadence, step length, joint angles, and GRFs—allow clinicians to detect subtle abnormalities. Understanding these metrics is essential when applying CO₂ cryotherapy, which can modify neuromuscular control and improve movement quality. Gait analysis helps measure how interventions alter biomechanics, guiding more targeted, data-driven rehabilitation plans.
Understanding Muscle Load Distribution
Muscle load distribution refers to how different muscle groups share force demands during gait. It ensures smooth propulsion, joint stability, and efficient shock absorption. EMG studies reveal the importance of timing and intensity in muscle recruitment across gait phases. For instance, some muscles absorb impact at heel strike, while others drive propulsion at push-off. A balanced load prevents overuse injuries. However, injury, pain, or compensation often disrupts this balance. A common example: reduced ankle dorsiflexion may cause overuse of hip flexors to compensate during swing, creating strain elsewhere. Chronic load imbalance can impair coordination and lead to long-term dysfunction. CO₂ cryotherapy provides a way to modulate overactive or underactive muscles, influencing motor control without fatigue. By temporarily changing muscle tone and proprioceptive input, clinicians can retrain patients toward more efficient load sharing. This makes it a valuable tool in addressing asymmetries and restoring functional movement patterns.
How CO₂ Cryotherapy Impacts Gait and Load Patterns
The therapeutic effects of CO₂ cryotherapy on gait and muscle load distribution result from complex interactions between temperature-induced physiological changes and neuromuscular adaptation mechanisms. These effects occur through multiple pathways that collectively alter movement patterns in measurable and clinically significant ways.
Immediate Neuromuscular Effects: Muscle Activation and Pain Modulation
CO₂ cryotherapy rapidly alters neuromuscular function by cooling tissues and slowing nerve conduction, leading to reduced pain and muscle hyperactivity. This temporary neuromodulation helps reset abnormal gait patterns. Pain relief occurs as cold slows nociceptive signals, enabling improved range of motion and reduced guarding—crucial for freer, more efficient movement. Muscle spindle sensitivity decreases, which lowers muscle tone in overactive areas. For example, applying CO₂ to a hypertonic gastrocnemius can enhance ankle dorsiflexion and improve heel-to-toe gait progression. Timing of muscle activation may also shift due to nerve conduction changes, offering a chance to retrain delayed or premature contraction patterns that impair gait coordination. These immediate effects make CO₂ cryotherapy an ideal tool for dynamic, phase-specific gait correction.
Rebalancing Muscle Load
CO₂ cryotherapy enables strategic muscle load redistribution by targeting overactive muscle groups. This approach reduces dominance in hypertonic areas, allowing weaker or underused muscles to engage more effectively. For instance, applying CO₂ to the overactive tensor fasciae latae can help activate the underutilized gluteus medius, enhancing lateral hip stability. This rebalancing supports reciprocal inhibition, where reduced tone in one muscle enhances its antagonist’s activity. Additionally, CO₂ therapy helps reset muscle activation sequences, promoting more synchronized movement. These benefits are especially useful in addressing gait deficits from poor coordination rather than weakness alone. Over time, repeated cryotherapy sessions paired with functional training may produce lasting improvements in motor control, reducing compensatory strategies and enabling more even force distribution during movement.
Altered Ground Reaction Forces (GRF)
Ground reaction forces (GRFs) reflect how the body interacts with the ground during movement. CO₂ cryotherapy alters muscle activation and joint control, which can reduce peak GRFs and improve loading symmetry. Targeting key muscles—like the quads, glutes, or plantarflexors—improves shock absorption during initial contact and enhances force generation during push-off. Temporal changes in GRF patterns reflect improved gait efficiency and reduced joint stress, particularly important in injury rehabilitation or osteoarthritis. Mediolateral GRFs also benefit when stabilizing muscles (e.g., hip abductors) are modulated, helping reduce energy-wasting lateral sway and prevent falls. Perhaps most significantly, CO₂ cryotherapy improves GRF symmetry between limbs, a key factor in restoring balanced gait in patients post-surgery, stroke, or with chronic asymmetries. These effects can be observed in real time using gait analysis systems, offering measurable progress indicators.
Neuromuscular Feedback and Proprioception
Proprioception—the body’s ability to sense position and movement—is deeply tied to balance and coordination. CO₂ cryotherapy can influence proprioceptive inputs by reducing muscle guarding and sensory noise, which in turn improves motor clarity and movement accuracy. Though cryotherapy may initially blunt some sensory feedback, the reduction in pain and tension allows for improved functional proprioception during gait. This supports better balance responses and reduces fall risk in populations with impaired motor control. CO₂ cryotherapy may also affect central neuromodulators like dopamine and sympathetic nervous system activity, enhancing the brain’s ability to learn or rewire movement patterns. Practitioners can strategically time gait retraining or balance drills during periods of heightened motor learning and proprioceptive receptivity following treatment. This effect is particularly valuable in neurorehabilitation and sports retraining, where restoring timing and coordination is as crucial as improving strength or mobility.
Clinical and Sports Use Cases
The practical applications of CO₂ cryotherapy for gait modification and load distribution improvement span numerous clinical and athletic scenarios. Understanding specific use cases and their expected outcomes helps practitioners develop targeted treatment protocols and set appropriate expectations for patients and athletes.
Post-Operative Rehabilitation
Post-operative gait recovery is often hindered by pain, inflammation, and muscle inhibition. CO₂ cryotherapy offers a targeted solution by reducing pain, swelling, and protective movement patterns without stressing healing tissues. It is particularly effective after procedures like total knee arthroplasty, where improved range of motion and early mobility are essential. By rapidly lowering pain levels, CO₂ cryotherapy enables patients to practice normalized gait during a critical recovery window, helping prevent long-term compensations. It also addresses quadriceps inhibition, a common issue after surgery, by relaxing overactive opposing muscles and reducing nociceptive interference—facilitating better muscle recruitment. Furthermore, CO₂ cryotherapy’s anti-inflammatory effects support tissue healing while preserving joint mobility and neuromuscular coordination. When used alongside physical therapy, it enhances functional recovery by targeting both physiological and mechanical contributors to poor post-operative gait.
Sports Injury Recovery
Athletes recovering from injury need fast, precise interventions to regain movement efficiency and prevent re-injury. CO₂ cryotherapy is well-suited for this, as it can rapidly alter muscle activation patterns, reduce inflammation, and correct faulty biomechanics—key for both overuse and acute injuries. In overuse cases, CO₂ helps athletes experience improved movement strategies by temporarily altering neuromuscular timing. When paired with motion feedback, it enables real-time gait retraining. In acute injuries, it allows continued movement with reduced risk by managing pain and preserving neuromotor control. As athletes progress through return-to-play protocols, CO₂ therapy can remove residual movement restrictions, accelerating adaptation to increasing load demands. Some elite athletes even use it pre-training for performance priming, leveraging its effects on neuromuscular responsiveness and coordination for enhanced movement economy.
Chronic Pain & Movement Disorders
Chronic pain and movement disorders often involve compensatory motor patterns, muscle hypertonia, and heightened sensitivity. CO₂ cryotherapy offers a brief but powerful intervention that addresses localized pain, muscle tone, and movement quality simultaneously. For conditions like fibromyalgia, the treatment’s short duration and targeted application are well-tolerated, making it ideal for individuals who struggle with traditional therapies. In spasticity or dystonia, cold exposure may temporarily reduce excessive tone, helping improve mobility and comfort during therapy. Neurological gait disorders benefit from CO₂’s ability to reduce spasticity, normalize muscle recruitment, and enhance proprioceptive clarity. However, its temporary nature requires integration with structured therapy for long-term gains. In chronic low back pain, where gait adaptations often aggravate symptoms, applying CO₂ to lumbopelvic and hip stabilizers can help restore normal load sharing, reduce compensation, and support spinal health—addressing the root mechanical contributors to persistent pain.
Tools & Technology: Measuring the Impact
Accurate assessment of CO₂ cryotherapy’s effects on gait and muscle load distribution requires sophisticated measurement technologies and standardized protocols. These tools not only provide objective evidence of treatment efficacy but also guide treatment modifications and help establish evidence-based practice guidelines.
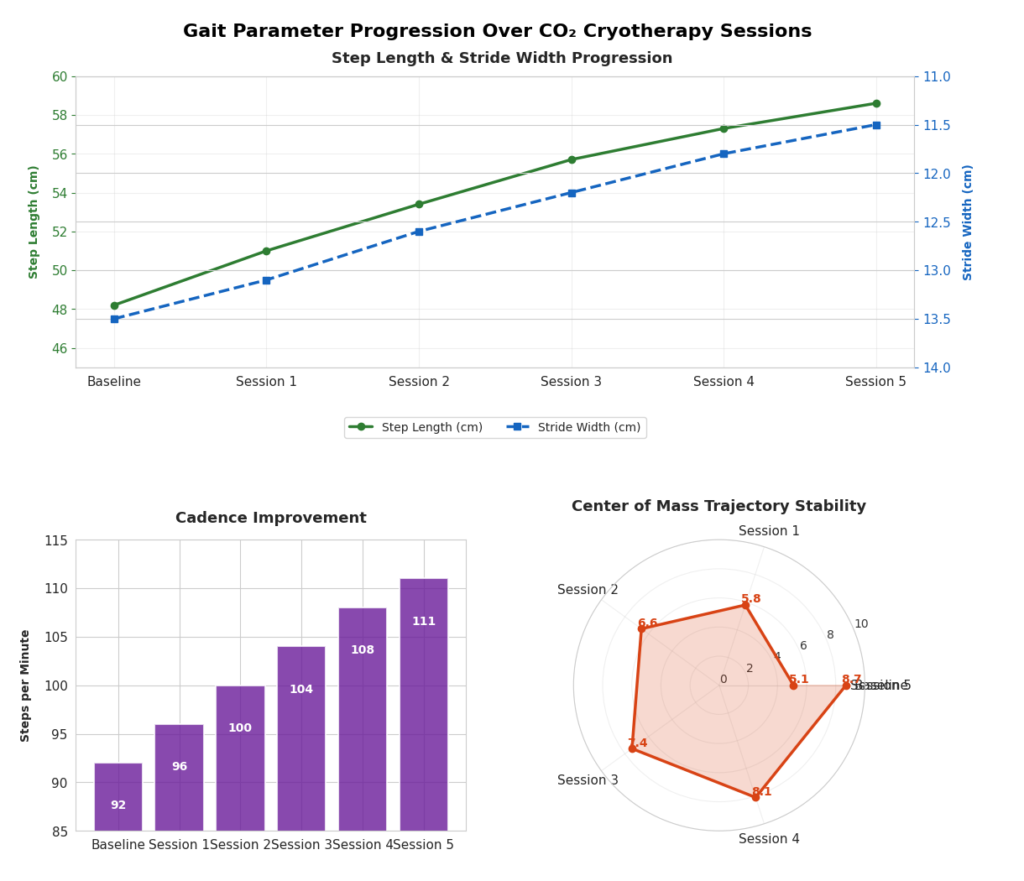
Motion Tracking and Gait Analysis Technologies: Measuring Cryotherapy Outcomes
Modern motion analysis systems, including 3D marker-based/markerless technologies, allow precise measurement of joint kinematics and gait parameters after CO₂ cryotherapy. Clinically relevant spatial-temporal metrics—step length, cadence, stance time—can reflect improvements in pain, balance, and gait efficiency. These can be assessed via force plates or pressure-sensitive walkways. Joint-specific changes, such as increased ankle dorsiflexion or improved hip extension, are measurable and highlight movement normalization post-treatment. Center of mass trajectories and dynamic stability indicators also reflect gains in balance and neuromuscular coordination, especially in elderly or neurologically impaired patients. Wearable technologies like inertial measurement units (IMUs) and accelerometers make gait monitoring feasible in real-world settings, supporting long-term outcome tracking. These tools extend analysis beyond the clinic, allowing adjustments based on patients’ daily movement patterns and providing actionable insights into therapy efficacy over time.
EMG and Muscle Load Tracking
Surface EMG enables real-time analysis of muscle activation before and after CO₂ cryotherapy, revealing treatment-induced changes in timing, amplitude, and coordination. Shifts in activation onset or duration indicate altered neuromuscular control, often correlating with improvements in gait quality. Co-contraction patterns—especially between antagonistic muscles—offer insights into motor control efficiency. Reduced inappropriate co-contractions post-treatment suggest better muscular coordination and less protective guarding. EMG also detects changes in muscle fatigue through frequency analysis, with improvements often linked to enhanced endurance and energy efficiency. Combining EMG with motion analysis provides a comprehensive view of how muscle activity drives observed movement changes. This integration helps determine whether functional gains stem from normalized muscle recruitment or compensatory strategies, enabling clinicians to refine interventions with precision.
Clinical Protocols and Safety Considerations
Standardized protocols ensure safe, effective CO₂ cryotherapy use. Key parameters include gas temperature (-78°C), application duration (10–15 seconds), and precise anatomical targeting. Consistent delivery is supported by well-calibrated equipment and trained practitioners. Pre-treatment screening is essential—clinicians must assess for contraindications like poor circulation, skin integrity issues, or sensory deficits. Proper patient positioning and stabilization minimize safety risks and maximize treatment accuracy. Safety procedures include continuous monitoring during application and clear emergency protocols. Post-treatment assessments (skin condition, sensation, joint mobility) help detect adverse reactions and track immediate benefits. Longitudinal follow-up ensures functional gains are maintained. Comprehensive documentation—including treatment details and patient responses—facilitates clinical auditing and research. Integration with electronic health records supports protocol refinement and contributes to developing evidence-based best practices.
Expert Perspectives and Evidence-Based Support
Experts emphasize that CO₂ cryotherapy’s success hinges on precise technique and proper patient selection. Its effects are highly specific, requiring in-depth knowledge of neuromuscular physiology, anatomy, and biomechanics. While immediate benefits like pain relief, improved muscle activation, and joint mobility are well-supported by research, long-term impacts on movement patterns need further study. Current evidence suggests CO₂ cryotherapy enhances neuromuscular recovery and facilitates therapeutic windows for movement retraining and manual therapy. These transient improvements allow patients to perform activities otherwise hindered by pain or guarding. However, cryotherapy should complement—not replace—broader rehabilitation strategies. Adoption challenges include equipment costs and the need for advanced training. Still, its precision may reduce overall treatment time and improve outcomes. Experts call for further studies on optimal dosing, long-term effects, and its role alongside other therapies. Such research will shape the strategic integration of CO₂ cryotherapy into evidence-based rehabilitation protocols.
Conclusion

CO₂ cryotherapy offers a unique, targeted tool for improving gait and neuromuscular function through precise, rapid-acting interventions. It addresses underlying dysfunctions rather than merely masking symptoms, enabling faster recovery in post-operative rehab, sports injuries, and chronic pain conditions. Its benefits stem from physiological changes triggered by extreme cold—modulating muscle tone, reducing pain, and improving joint function. These effects create critical windows for retraining movement patterns, enhancing therapy outcomes when used alongside manual or exercise-based approaches. Motion analysis and EMG are essential in objectively validating treatment effects and guiding personalized protocols. As clinical experience grows and evidence accumulates, CO₂ cryotherapy is poised to become a mainstay in movement rehabilitation. Future directions include refining protocols, expanding access through technological innovation, and aligning treatments with patient-specific goals. By embracing ongoing research and clinical innovation, practitioners can maximize the potential of CO₂ cryotherapy to elevate movement quality and restore function in diverse patient populations.
FAQs
CO₂ cryotherapy uses pressurized carbon dioxide gas at -78°C for rapid, targeted cooling. Unlike ice packs, it penetrates deeper tissues quickly without prolonged application time, allowing for more precise neuromuscular effects and faster treatment sessions.
Yes, when applied correctly by trained professionals, CO₂ cryotherapy is safe post-surgery. It reduces pain and swelling without stressing healing tissues. However, screening for skin integrity and circulation issues is essential before use.
Yes. It offers rapid pain relief and can reduce muscle hypertonia, enabling better movement patterns during therapy. While effects are temporary, they create a window for functional retraining and improved quality of life.
Many patients experience immediate effects such as reduced pain and improved mobility after a single session. Long-term gait improvements, however, depend on repeated applications combined with physical therapy.
Yes. It aids in recovery from overuse and acute injuries by reducing inflammation and optimizing movement patterns. Some athletes also use it pre-competition to enhance neuromuscular readiness and efficiency.
Yes. Treatment requires a medical-grade CO₂ delivery device with precise temperature and spray control. Trained clinicians should operate the equipment to ensure safety and therapeutic accuracy.



