Introduction
Circulation and tissue oxygenation are critical physiological processes that support cellular metabolism, nutrient delivery, waste removal, and overall tissue health. When blood flow or oxygen delivery is compromised, tissue recovery slows, pain may increase, and the risk of chronic dysfunction rises. CO₂ cryotherapy—a specialized form of cold therapy using carbon dioxide gas at controlled low temperatures—has emerged as an innovative, non-invasive approach that may positively influence microcirculation and tissue oxygenation. This article explores the science behind CO₂ cryotherapy, how it differs from traditional cold therapy methods, and why it has the potential to enhance blood flow and oxygenation in targeted tissues.
1. Understanding Circulation and Tissue Oxygenation
Before discussing how CO₂ cryotherapy exerts its effects, it is essential to understand the underlying physiological processes of circulation and tissue oxygenation. Blood flow and oxygen transport are fundamental to all aspects of tissue function, repair, and recovery.
1.1 What Is Blood Circulation and Why It Matters
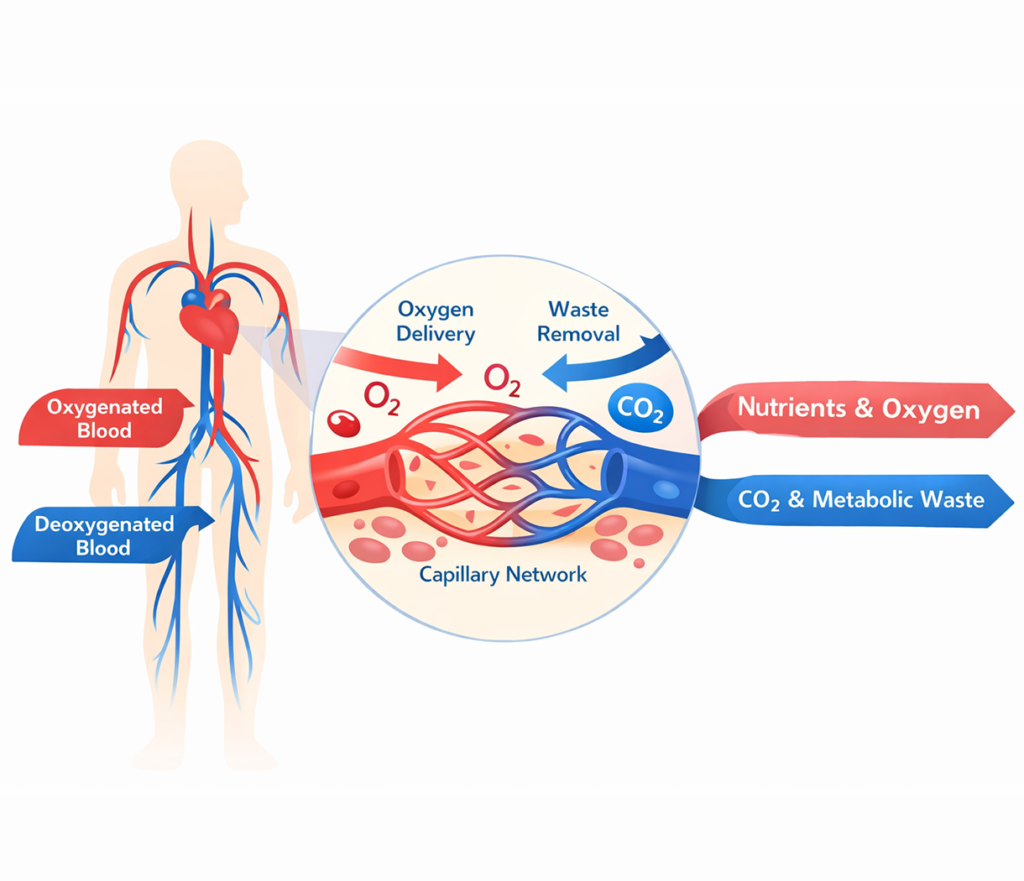
Blood circulation is the continuous, rhythmic movement of blood through the body’s cardiovascular system, driven by the pumping action of the heart and moderated by the vascular network of arteries, veins, and capillaries. Arteries carry oxygen-rich blood from the heart to the organs and tissues, while veins return deoxygenated blood back to the lungs for oxygen replenishment.
Efficient circulation is more than just the delivery of oxygen; it also ensures the transport of essential nutrients, hormones, and immune cells to sites of injury or metabolic demand. Furthermore, circulation plays a pivotal role in removing metabolic waste products such as carbon dioxide and lactic acid. Impaired circulation can manifest as fatigue, delayed healing, pain, or neuropathy, especially in regions prone to mechanical stress or inflammation.
1.2 Tissue Oxygenation and Cellular Metabolism
Tissue oxygenation refers to the level of oxygen available within tissues for cellular metabolism. Oxygen is vital for aerobic energy production via oxidative phosphorylation in mitochondria, which generates ATP (adenosine triphosphate), the primary energy currency of cells. When tissues are well‑oxygenated, cellular processes function efficiently, leading to effective repair, reduced inflammation, and improved overall function.
In contrast, hypoxic (low oxygen) conditions can compromise cellular metabolism, increase oxidative stress, and trigger maladaptive inflammatory responses. In musculoskeletal injuries or chronic pain conditions, prolonged hypoxia may delay healing and exacerbate symptoms. Therefore, strategies that improve local oxygen delivery can have meaningful therapeutic benefits.
2. What Is CO₂ Cryotherapy?
CO₂ cryotherapy is a form of local cryotherapy that uses carbon dioxide gas expelled at high velocity and low temperature to cool targeted tissues. It differs from traditional cold therapy methods by offering precise temperature control, deeper skin penetration, and distinct physiological reactions.
2.1 How CO₂ Cryotherapy Works
CO₂ cryotherapy systems typically deliver carbon dioxide gas at temperatures ranging from −78 °C to −90 °C (dry ice equivalent) through a specialized nozzle applied near the skin surface. As the cold gas contacts the skin, it induces rapid cooling of superficial tissues. Unlike ice packs or cold water immersion, CO₂ cryotherapy provides uniform and controlled temperature reduction without moisture or prolonged pressure.
On a cellular level, this rapid cooling triggers a sequence of vascular and neurological responses. Initially, cold exposure causes vasoconstriction—tightening of local blood vessels—as the body conserves heat and protects core temperature. Once the stimulus is removed, a phenomenon known as reactive hyperemia occurs, where blood vessels dilate (vasodilation) and increase blood flow to the previously cooled area. This vascular rebound effect is central to enhanced circulation and can improve nutrient and oxygen delivery to tissues.
2.2 CO₂ Cryotherapy vs Traditional Cold Therapy
Traditional cold therapy methods like ice packs, cold water immersion, or gel packs produce therapeutic cooling primarily through conduction and convection. While these methods are effective in reducing pain and swelling in acute injury settings, they lack the precision and depth control offered by CO₂ cryotherapy. Ice packs may cause uneven cooling, skin maceration, or frostbite if left too long, and cold water immersion is impractical for localized treatment in many settings.
By contrast, CO₂ cryotherapy delivers a controlled, dry, and reproducible temperature profile that can be tailored to individual needs. Because carbon dioxide gas is dry and rapidly evaporates, it minimizes moisture‑related skin issues and allows for a more comfortable patient experience. This makes CO₂ cryotherapy particularly useful in clinical, rehabilitation, and athletic performance settings.
3. Physiological Effects of CO₂ Cryotherapy on Circulation
CO₂ cryotherapy affects circulation through a complex interplay of vascular and neurological responses. These changes can help improve local blood flow, enhance microcirculation, and ultimately support tissue healing and metabolic activity.
3.1 Vasoconstriction and Vasodilation Response
When cold is applied to the skin, superficial blood vessels initially constrict to reduce heat loss. This vasoconstriction response is a protective mechanism. However, as soon as the cold stimulus is removed, the body initiates a reflexive vasodilation—expanding the diameter of blood vessels in the treated area. This rebound effect leads to a significant increase in local blood flow, compared with baseline levels before treatment.
This sequence, often described in cryotherapy literature, represents a physiological “pump” that enhances blood circulation. Reactive vasodilation allows oxygenated blood and immune cells to reach the cooled tissues more efficiently, facilitating waste removal and supporting repair processes. Over repeated sessions, this improved microvascular function may contribute to long‑term tissue health.
3.2 Enhanced Microcirculation After Treatment
Microcirculation refers to blood flow within the smallest vessels—arterioles, capillaries, and venules—that directly interface with tissues. Enhanced microcirculation ensures that oxygen and nutrients are delivered right where they are needed most at the cellular level. CO₂ cryotherapy appears to facilitate improvements in microcirculatory perfusion by triggering a controlled temperature gradient that stimulates vascular responsiveness and endothelial function.
Endothelial cells lining blood vessels respond to changes in temperature and shear stress by releasing vasodilatory mediators such as nitric oxide (NO). Increased nitric oxide availability further supports vasodilation, ultimately improving capillary blood flow and oxygen delivery. These responses may benefit tissues experiencing inflammation, ischemia, or mechanical stress.
4. CO₂ Cryotherapy and Tissue Oxygenation
Improved circulation naturally leads to enhanced oxygen delivery and utilization within tissues. This section describes how CO₂ cryotherapy can positively influence these processes.
4.1 Improved Oxygen Delivery to Treated Areas
Once blood flow is enhanced through reactive vasodilation and improved microcirculation, the next critical step is oxygen delivery. Oxygen is transported bound to hemoglobin in red blood cells and released into tissues based on local metabolic demand and perfusion pressure. By increasing blood flow velocity and capillary recruitment, CO₂ cryotherapy allows more oxygen‑rich blood to access areas that may have been relatively hypoxic due to injury, inflammation, or poor circulation.
Improved oxygen availability supports several beneficial processes, including increased ATP production, enhanced leukocyte function, and reduced anaerobic metabolism. These changes can reduce oxidative stress and lower lactic acid accumulation, leading to improved tissue recovery and reduced pain.
4.2 Effects on Hypoxic or Inflamed Tissues
Hypoxia (insufficient oxygen supply) and inflammation often go hand in hand in injured or compromised tissues. When local oxygen demand exceeds supply, tissue metabolism shifts toward less efficient anaerobic pathways, increasing byproducts that contribute to pain and swelling. By enhancing blood flow and oxygen delivery, CO₂ cryotherapy may help shift the microenvironment back toward aerobic metabolism, reducing inflammatory signaling and supporting cellular repair.
Tissues that are chronically inflamed or hypoxic may also exhibit impaired lymphatic function and nutrient exchange. Improved circulation following CO₂ cryotherapy may facilitate lymphatic drainage and reduce edema, further supporting recovery and functional restoration.
5. Clinical and Practical Benefits
The physiological effects of CO₂ cryotherapy on circulation and oxygenation translate into a range of practical benefits for individuals recovering from injury, experiencing pain, or seeking enhanced performance recovery.
5.1 Muscle Recovery and Fatigue Reduction
Muscle fatigue often results from metabolic byproduct accumulation, microtrauma to muscle fibers, and transient reductions in oxygen availability during intense activity. By enhancing blood flow and improving oxygen delivery post‑exercise, CO₂ cryotherapy can help clear metabolic waste more efficiently and reduce delayed onset muscle soreness (DOMS). Athletes and physically active individuals often report quicker recovery, reduced soreness, and improved readiness for subsequent activity when cryotherapy is integrated into training recovery protocols.
Improved perfusion also supports the restoration of calcium homeostasis within muscle fibers, which is critical for optimal contraction and relaxation cycles. Enhanced circulation may help reduce cramping and stiffness that can follow strenuous exercise.
5.2 Joint, Tendon, and Soft Tissue Support
Soft tissues like tendons, ligaments, and joint capsules often have limited vascular supply compared with muscle. This relative avascularity can slow healing and increase susceptibility to chronic inflammation. CO₂ cryotherapy’s ability to enhance local circulation can help overcome some of these limitations by increasing nutrient and oxygen delivery to these challenging areas.
In addition, improved microcirculation may help modulate pain signaling around joints and tendons. Enhanced blood flow supports macrophage activity and collagen synthesis, processes that are essential for tendon repair and connective tissue remodeling. For individuals with tendinopathies or joint pain without structural damage, improved perfusion may provide meaningful symptom relief.
6. Who May Benefit Most from Improved Circulation via CO₂ Cryotherapy
Not all individuals are ideal candidates for every therapy, but certain populations may derive particular benefit from the circulatory and oxygenation enhancements associated with CO₂ cryotherapy.
6.1 Athletes and Physically Active Individuals
Athletes, cross‑fit participants, runners, and weight lifters place repeated mechanical stress on muscles and joints. This stress can lead to microtrauma, inflammation, and transient reductions in local oxygen delivery. Incorporating CO₂ cryotherapy into post‑training or post‑competition recovery routines may accelerate the resolution of inflammation and promote faster tissue repair, allowing more frequent high‑quality training sessions.
For athletes with overuse injuries or chronic tendon pain, improved microcirculation can support long‑term healing and reduce reliance on pain medications or invasive interventions. It can also serve as a preventative strategy during heavy training cycles.
6.2 Patients with Circulation‑Related Pain or Recovery Challenges
Individuals with chronic pain syndromes—particularly those with poor peripheral circulation due to sedentary lifestyle, metabolic conditions, or aging—may also benefit from cryotherapy’s circulatory effects. For example, patients with non‑specific low back pain, myofascial pain syndromes, or post‑operative rehabilitation needs may experience improved comfort and functional outcomes when enhanced blood flow and oxygen delivery support the body’s own healing processes.
In these populations, better circulation can also help reduce muscle stiffness, improve range of motion, and decrease reliance on systemic pain medications with potential side effects.
7. Safety Considerations and Treatment Expectations
While CO₂ cryotherapy offers promising benefits, it is important to understand safety considerations, contraindications, and realistic treatment expectations.
7.1 Is Improving Circulation with CO₂ Cryotherapy Safe?
CO₂ cryotherapy is generally considered safe when performed according to established protocols. The rapid cooling of superficial tissues is well tolerated by most individuals, but proper temperature control and trained administration are essential to avoid cold‑induced skin injury such as frostbite or cold urticaria. Individuals with peripheral vascular disease, Raynaud’s phenomenon, open wounds, or certain neuropathies should consult with healthcare professionals before undergoing cryotherapy.
Practitioners trained in its application can adjust duration, distance, and cooling intensity to minimize risk and maximize therapeutic benefits. As with any therapeutic intervention, patient screening and monitoring improve safety and outcomes.
7.2 Treatment Frequency and Expected Outcomes
CO₂ cryotherapy sessions are typically brief, ranging from 2–10 minutes per treated area, and may be performed multiple times per week depending on the condition being addressed. Early circulatory benefits—such as improved warmth, reduced stiffness, and enhanced movement—may be noticeable after a few sessions, while cumulative benefits on oxygenation and recovery often require consistent application over several weeks.
Combining cryotherapy with other interventions—such as physical therapy, graded exercise, and ergonomic adjustments—can further enhance outcomes and support long‑term improvements in function and comfort.
FAQ
Does CO₂ cryotherapy increase or decrease blood flow?
CO₂ cryotherapy initially induces vasoconstriction due to rapid cooling, followed by reactive vasodilation once the cold stimulus is removed. This rebound effect increases local blood flow and supports enhanced oxygen delivery to tissues.
How long do circulation benefits last after a session?
Circulation improvements can persist for hours to days following treatment, depending on individual vascular responsiveness and the frequency of sessions. Repeated treatments may promote sustained microvascular function.
Can CO₂ cryotherapy help with poor circulation?
By improving local microcirculation and supporting vascular responsiveness, CO₂ cryotherapy may benefit individuals with localized circulation challenges, especially when integrated into a broader therapeutic plan.
Is CO₂ cryotherapy suitable for older adults?
Many older adults can safely undergo cryotherapy with appropriate screening and professional supervision. However, pre‑existing conditions such as peripheral vascular disease or neuropathy require careful evaluation before treatment.
Conclusion
CO₂ cryotherapy represents a modern cold therapy modality that goes beyond simple surface cooling. By inducing controlled vascular responses, enhancing microcirculation, and supporting improved tissue oxygenation, it offers practical benefits for muscle recovery, pain modulation, and rehabilitation. Athletes, physically active individuals, and patients with circulation‑related recovery challenges may all find value in cryotherapy as part of a comprehensive treatment approach. As with any therapeutic intervention, safety considerations and individualized treatment plans are essential for maximizing benefits and minimizing risks.
References
Bleakley, C. M., & Davison, G. W. What is the biochemical and physiological rationale for using cold‑water immersion in sports recovery? Sports Med.
https://pubmed.ncbi.nlm.nih.gov/23379514/
Costello, J. T., Baker, P. R., & Minett, G. M. Whole‑body cryotherapy (extreme cold air exposure) for preventing and treating muscle soreness after exercise in adults. Cochrane Database Syst Rev.
Swenson, C., Sward, L., & Karlsson, J. Cryotherapy in sports injury management. Sports Med.
https://pubmed.ncbi.nlm.nih.gov/7787939/
Costello, J. T., Algar, L. A., & Donnelly, A. E. Effects of whole‑body cryotherapy (-110 °C) on proprioception and indices of muscle damage. Scand J Med Sci Sports.
https://pubmed.ncbi.nlm.nih.gov/20840270/
Ferreira‑Junior, J. B., Tenório, T. R. L., Gonçalves, L. G. B., et al. Evaluation of microcirculation after cryotherapy application. J Therm Biol.
https://www.sciencedirect.com/science/article/pii/S0306456518303670


