소개
Modern therapeutic approaches increasingly focus on enhancing vascular health as a cornerstone of recovery and pain management. Among emerging technologies, CO₂ cryotherapy represents a paradigm shift in how we approach circulatory enhancement through controlled thermal therapy.
Why Vascular Health Matters in Pain and Recovery
Vascular health serves as the foundation for effective pain management and tissue recovery. The circulatory system’s primary function involves delivering oxygen and nutrients while removing metabolic waste products from tissues. When circulation becomes compromised, whether through injury, inflammation, or chronic conditions, the body’s natural healing mechanisms become impaired. Poor circulation contributes to prolonged recovery times, increased pain sensation, and delayed tissue repair. Understanding this fundamental relationship between vascular function and therapeutic outcomes has driven researchers and clinicians to develop targeted interventions that specifically address circulatory deficits in treatment protocols.
The Rise of CO₂ Cryotherapy in Modern Therapeutics
Cryotherapy has been spreading in various wellness initiatives, integrating with other treatments to enhance overall health, improve circulation, reduce inflammation, and promote relaxation. CO₂ cryotherapy represents an evolution from traditional cold therapy methods, offering precise temperature control and targeted application. Unlike conventional ice packs or whole-body cryotherapy chambers, CO₂ systems deliver controlled cooling through 가압 이산화탄소 가스. This technology emerged from dermatological applications and has expanded into sports medicine, rehabilitation, and pain management. The precision and consistency of CO₂ delivery systems allow healthcare providers to achieve therapeutic temperatures of -78°C within seconds, creating predictable physiological responses that traditional methods cannot match consistently.
Exploring the Circulatory Impact of CO₂ Cryotherapy
The vascular effects of CO₂ cryotherapy extend beyond simple vasoconstriction and encompass complex physiological cascades that influence both local and systemic circulation. The benefits of cryotherapy are due to a combination of physiological responses, including vasoconstriction, decreased vasodilation, increased endorphins and collagen production, increased circulation, reduced inflammation, increased mitochondrial activity, enhanced tissue repair. This comprehensive approach to circulatory enhancement makes CO₂ cryotherapy particularly valuable for conditions requiring rapid vascular response and sustained therapeutic benefits. The unique characteristics of CO₂ as a therapeutic medium create distinct advantages in terms of penetration depth, treatment duration, and physiological response compared to other cryotherapy modalities.
CO₂ 냉동 요법 이해
The foundation of effective CO₂ cryotherapy lies in understanding its unique mechanisms and applications. This advanced therapeutic modality combines principles of thermodynamics, vascular physiology, and controlled drug-free pain management to achieve targeted treatment outcomes.
CO₂ 냉동 요법이란 무엇인가요?
CO₂ cryotherapy utilizes pressurized carbon dioxide gas to create controlled, localized cooling effects on targeted tissues. The system operates by releasing CO₂ through specialized applicators, achieving therapeutic temperatures of -78°C within 10-15 seconds of application. This rapid temperature reduction creates a thermal shock effect that triggers immediate physiological responses in both superficial and deeper tissue layers. The CO₂ gas transitions from liquid to gas phase during application, creating an endothermic reaction that efficiently absorbs heat from the treatment area. This process differs significantly from traditional cold therapy methods, as it provides consistent temperature delivery without the variability associated with ice packs or cold compresses.
How CO₂ Cryotherapy Works on the Skin and Vascular System
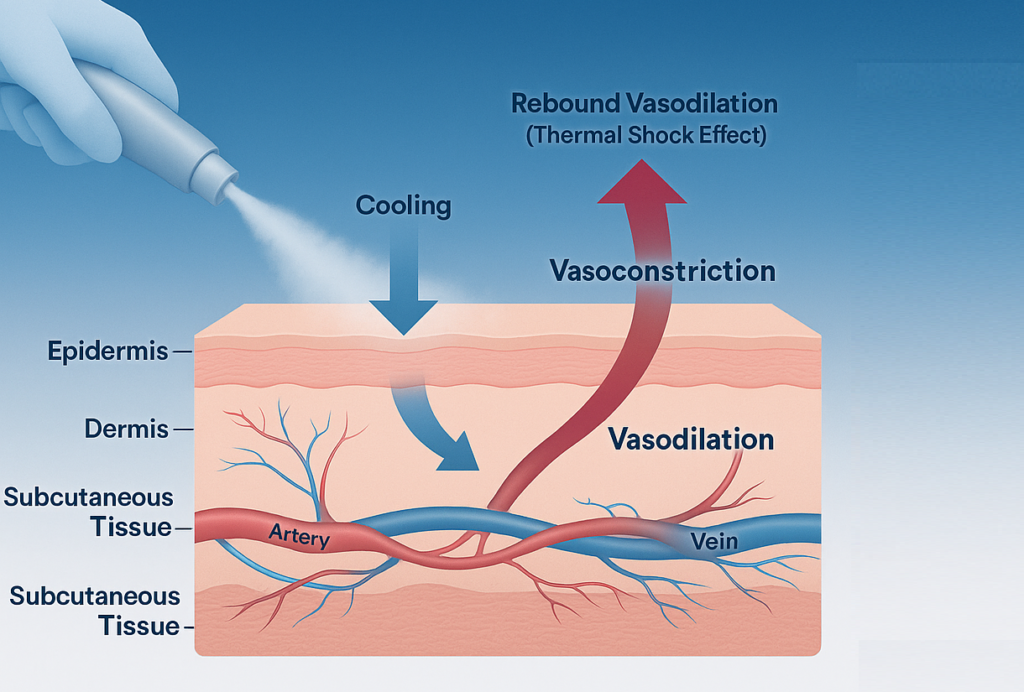
The application of CO₂ cryotherapy initiates a cascade of vascular responses beginning at the epidermal level and extending into deeper tissue structures. Upon contact with -78°C CO₂, the skin experiences immediate vasoconstriction as smooth muscle cells in arterioles contract in response to thermal stimuli. This initial response activates thermoreceptors and nociceptors, triggering neurogenic reflexes that influence local blood flow patterns. The rapid temperature change stimulates the release of vasoactive substances, including nitric oxide and endothelin, which modulate vascular tone. Simultaneously, the cold exposure activates the sympathetic nervous system, leading to systemic cardiovascular adjustments that complement the local vascular effects. The controlled duration of 10-15 seconds ensures therapeutic benefit while preventing tissue damage.
Difference Between CO₂ Cryotherapy and Other Modalities
CO₂ cryotherapy offers distinct advantages over traditional cryotherapy methods in terms of temperature control, application precision, and therapeutic consistency. Unlike ice packs that gradually lose effectiveness and create uneven cooling patterns, CO₂ systems maintain constant therapeutic temperatures throughout the treatment duration. Whole-body cryotherapy chambers expose patients to -110°C to -140°C for 2-3 minutes, creating systemic effects but lacking the targeted precision of localized CO₂ application. Liquid nitrogen cryotherapy, while achieving similar temperatures, poses greater safety risks and requires specialized handling protocols. CO₂ cryotherapy combines the therapeutic benefits of extreme cold with enhanced safety profiles, precise targeting capabilities, and consistent delivery mechanisms that make it suitable for both clinical and home-use applications.
The Vascular Response to CO₂ Cryotherapy
The vascular system’s response to CO₂ cryotherapy involves complex physiological mechanisms that create both immediate and sustained therapeutic benefits. Understanding these responses provides insight into the clinical applications and optimal treatment protocols for various conditions.
Immediate Vasoconstriction and Rebound Vasodilation
The initial vascular response to CO₂ cryotherapy involves rapid vasoconstriction mediated by both direct thermal effects and neurogenic reflexes. This manifests itself mainly as superficial skin vasospasm, increased vascular resistance and increased venous return, resulting in an increase in blood pressure. The immediate cooling effect triggers alpha-adrenergic receptors in vascular smooth muscle, causing arteriolar constriction that reduces local blood flow by 60-80% within seconds of application. This vasoconstriction serves protective functions by minimizing heat loss and reducing inflammatory mediator delivery to the treatment area. Following the initial constriction phase, a predictable rebound vasodilation occurs as the tissue rewarms, creating a hyperemic response that enhances circulation beyond baseline levels.
The “Thermal Shock” Effect Explained
The thermal shock effect represents the physiological response to rapid temperature changes that exceed the body’s normal adaptive capacity. When tissues experience a sudden drop from normal body temperature (37°C) to -78°C, cellular and vascular structures undergo immediate adaptive responses. This thermal gradient activates cold-sensitive ion channels, particularly TRPM8 and TRPA1 receptors, which initiate cellular signaling cascades affecting vascular tone. The shock response triggers the release of heat shock proteins, which protect cellular structures while promoting vascular adaptation. Additionally, the rapid temperature change stimulates the release of catecholamines, creating systemic effects that complement local vascular responses and contribute to the overall therapeutic benefit.
Localized Vascular Adaptation
Localized vascular adaptation following CO₂ cryotherapy involves structural and functional changes in the microcirculation that extend beyond the immediate treatment period. The initial vasoconstriction followed by reactive hyperemia creates a “vascular exercise” effect that improves endothelial function and capillary recruitment. This adaptation process involves upregulation of endothelial nitric oxide synthase (eNOS), increased production of vasodilatory prostacyclin, and improved vascular smooth muscle responsiveness. The repeated exposure to controlled thermal stress enhances the vessels’ ability to respond to future physiological demands, creating a conditioning effect similar to exercise training. These adaptations contribute to improved local circulation patterns and enhanced tissue oxygenation capacity.
Microcirculation Stimulation: Oxygenation and Nutrient Delivery
CO₂ cryotherapy significantly impacts microcirculatory function through multiple mechanisms that enhance tissue oxygenation and nutrient delivery. The post-treatment hyperemic response increases capillary perfusion pressure, improving the driving force for oxygen and nutrient transport across capillary walls. The cold-induced vasoconstriction followed by vasodilation creates a “milking” effect that enhances lymphatic drainage and venous return, reducing tissue edema that can impair microcirculatory function. Additionally, the thermal stimulation increases capillary recruitment, activating previously dormant capillaries and expanding the effective surface area for gas and nutrient exchange. Studies have investigated the effect of cryotherapy with carbon dioxide on muscle blood circulation, demonstrating measurable improvements in tissue perfusion following treatment protocols.
Angiogenesis and Long-Term Vascular Benefits
Repeated CO₂ cryotherapy applications stimulate angiogenesis through controlled activation of hypoxia-inducible factors and vascular growth factors. The initial reduction in tissue oxygenation during vasoconstriction triggers cellular hypoxia responses that upregulate vascular endothelial growth factor (VEGF) production. This growth factor stimulates endothelial cell proliferation and new vessel formation, enhancing the vascular network’s density and functional capacity. The thermal stress also activates heat shock proteins that protect existing vessels while promoting adaptive remodeling. Long-term benefits include improved collateral circulation, enhanced vascular reserve capacity, and increased resistance to ischemic injury. These adaptations make CO₂ cryotherapy particularly valuable for conditions involving compromised circulation or delayed healing responses.
Lymphatic Drainage Enhancement and Edema Reduction
The lymphatic system responds favorably to CO₂ cryotherapy through mechanisms that enhance fluid drainage and reduce tissue edema. The initial vasoconstriction reduces capillary filtration pressure, decreasing the formation of interstitial fluid. Subsequently, the rebound vasodilation creates pressure gradients that facilitate lymphatic uptake and drainage. The cold application also stimulates lymphatic smooth muscle contraction through direct thermal effects and neurogenic reflexes, improving lymphatic pumping efficiency. This enhanced drainage capacity reduces tissue swelling, improves cellular function, and creates favorable conditions for healing and recovery. The reduction in edema also decreases tissue pressure, which can improve local circulation and reduce pain sensation.
Improved Capillary Permeability and Cellular Exchange
CO₂ cryotherapy modulates capillary permeability through controlled effects on endothelial cell function and tight junction integrity. The initial vasoconstriction reduces hydrostatic pressure within capillaries, decreasing the driving force for fluid extravasation and inflammatory cell migration. The subsequent vasodilation phase enhances nutrient and oxygen delivery while maintaining controlled permeability that prevents excessive fluid accumulation. The thermal stress activates endothelial protective mechanisms, including increased production of barrier-stabilizing factors and improved tight junction protein expression. These effects optimize the balance between nutrient delivery and tissue protection, creating ideal conditions for cellular repair and regeneration processes.
Circulation in Seconds: What Makes CO₂ Cryotherapy Unique
The unique characteristics of CO₂ cryotherapy lie in its ability to create rapid, predictable vascular responses that distinguish it from other therapeutic modalities. These distinctive features enable precise control over circulatory effects and therapeutic outcomes.

Ultra-Fast Cooling and Vascular Reaction Time
CO₂ cryotherapy achieves therapeutic temperatures within 10-15 seconds, creating vascular reactions that occur almost instantaneously upon application. This rapid cooling rate exceeds the response time of traditional cold therapy methods by orders of magnitude, enabling precise control over treatment duration and intensity. The ultra-fast cooling activates vascular smooth muscle responses before compensatory mechanisms can fully engage, creating more predictable and consistent therapeutic effects. The immediate nature of the response allows practitioners to observe real-time treatment effects and adjust application parameters accordingly. This speed advantage makes CO₂ cryotherapy particularly valuable in acute injury management where rapid intervention can significantly impact outcomes.
Surface-to-Deep Tissue Penetration via Thermo Shock
The thermal shock created by CO₂ application penetrates beyond superficial tissues to affect deeper vascular structures through conductive and convective heat transfer mechanisms. Unlike surface cooling methods that primarily affect skin circulation, CO₂ cryotherapy creates thermal gradients that extend into subcutaneous tissues and underlying muscle layers. The rapid temperature change generates pressure waves that mechanically stimulate deep tissue mechanoreceptors, triggering vascular responses in structures not directly exposed to the cooling effect. This penetration depth enables treatment of conditions affecting deeper vascular networks while maintaining the precision and control of surface application. The multi-layered tissue response maximizes therapeutic benefit while minimizing treatment time and complexity.
How CO₂ Cryotherapy Enhances Endothelial Health and Nitric Oxide Production
CO₂ cryotherapy stimulates endothelial nitric oxide production through multiple pathways that enhance vascular health and function. The thermal stress activates endothelial nitric oxide synthase (eNOS) through calcium-dependent mechanisms, increasing NO production and improving vasodilatory capacity. The controlled hypoxia during vasoconstriction upregulates eNOS expression, creating sustained improvements in endothelial function beyond the immediate treatment period. Additionally, the shear stress generated during the vasodilation phase provides mechanical stimulation that further enhances NO production. These effects contribute to improved endothelial health, reduced oxidative stress, and enhanced vascular protective mechanisms. The combination of immediate and sustained NO enhancement makes CO₂ cryotherapy valuable for both acute treatment and long-term vascular health maintenance.
Balancing Vasodilation and Vasoconstriction for Optimal Circulation
The therapeutic effectiveness of CO₂ cryotherapy depends on achieving optimal balance between vasoconstriction and vasodilation phases to maximize circulatory benefits. The initial vasoconstriction phase reduces inflammatory mediator delivery and provides analgesic effects through reduced nerve conduction velocity. The subsequent vasodilation phase enhances nutrient delivery, promotes waste removal, and stimulates healing responses. The timing and magnitude of these responses can be controlled through treatment duration, temperature, and application frequency. This balance creates a “vascular training” effect that improves the circulatory system’s ability to respond to physiological demands. Optimal protocols consider individual patient factors, condition severity, and treatment goals to achieve the most beneficial vascular response patterns.
Systemic Circulatory Effects from Localized CO₂ Application
While CO₂ cryotherapy is applied locally, it creates systemic circulatory effects through neurogenic reflexes and hormonal responses. Such modulation of the autonomic nervous system is associated with faster post-exercise recovery. The local cold stimulation activates sympathetic nervous system responses that affect heart rate, blood pressure, and peripheral circulation beyond the treatment area. The release of catecholamines and other vasoactive substances creates systemic effects that complement local therapeutic responses. These systemic effects contribute to overall cardiovascular conditioning and may provide benefits for conditions affecting multiple body regions. The combination of local and systemic responses maximizes therapeutic efficiency while maintaining the safety and precision of targeted treatment approaches.
Clinical Applications of CO₂-Induced Vascular Stimulation
The diverse clinical applications of CO₂ cryotherapy reflect its versatility in addressing various conditions that benefit from improved circulation and controlled inflammatory responses. These applications span multiple medical specialties and treatment settings.
Sports Recovery and Muscle Oxygenation
CO₂ cryotherapy has become increasingly popular in sports medicine for enhancing recovery and improving muscle oxygenation following intense physical activity. Studies have investigated the effect of cryotherapy with carbon dioxide on fatigue recovery of neuromuscular function and muscle blood circulation. The rapid vasoconstriction followed by enhanced blood flow helps clear metabolic waste products, including lactate and inflammatory mediators that contribute to muscle fatigue and soreness. The improved oxygenation supports cellular energy production and accelerates protein synthesis necessary for muscle repair. Athletes report faster recovery times, reduced muscle stiffness, and improved performance readiness following CO₂ cryotherapy treatments. The precision targeting allows treatment of specific muscle groups without systemic effects that might interfere with training schedules.
Chronic Venous Insufficiency and Microvascular Disorders
Patients with chronic venous insufficiency benefit from CO₂ cryotherapy’s ability to improve venous return and reduce lower extremity edema. The vasoconstriction phase reduces venous pooling, while the subsequent vasodilation enhances arterial inflow and capillary perfusion. The improved lymphatic drainage helps manage chronic swelling and reduces the risk of complications associated with venous stasis. Microvascular disorders, including diabetic microangiopathy and peripheral arterial disease, show improvement with regular CO₂ cryotherapy applications. The enhanced capillary recruitment and improved endothelial function contribute to better tissue perfusion and reduced ischemic symptoms. Treatment protocols must be carefully adapted for patients with compromised circulation to ensure safety and optimize therapeutic outcomes.
Cold Therapy for Inflammation and Vascular Pain Relief
Local cryotherapy significantly reduced inflammatory markers, especially in microcrystal-induced arthritis, demonstrating its effectiveness in managing inflammatory conditions. CO₂ cryotherapy provides rapid pain relief through reduced nerve conduction velocity and decreased inflammatory mediator activity. The vasoconstriction phase limits inflammatory cell recruitment and reduces tissue edema that contributes to pain sensation. The controlled cooling effect desensitizes nociceptors and interrupts pain signal transmission, providing immediate relief for acute and chronic pain conditions. The anti-inflammatory effects extend beyond the treatment period, contributing to sustained pain reduction and improved functional outcomes. This dual action makes CO₂ cryotherapy particularly valuable for conditions where inflammation and pain significantly impact quality of life.
Wound Healing and Scar Tissue Remodeling
CO₂ cryotherapy supports wound healing through enhanced circulation, reduced inflammation, and stimulation of growth factor production. The improved blood flow delivers oxygen, nutrients, and immune factors necessary for tissue repair processes. The controlled inflammatory response promotes appropriate healing progression while preventing excessive scar formation. The thermal stimulation activates fibroblasts and promotes organized collagen deposition, improving wound strength and appearance. For existing scar tissue, CO₂ cryotherapy can promote remodeling through enhanced circulation and controlled inflammatory responses that break down excessive collagen deposits. The precision of application allows treatment of delicate areas while maintaining safety and effectiveness. Treatment protocols must be individualized based on wound characteristics, healing stage, and patient factors.
Scientific Evidence Supporting Vascular Effects
The growing body of scientific evidence supporting CO₂ cryotherapy’s vascular effects provides a strong foundation for its clinical applications and continued development. Research findings from multiple disciplines contribute to our understanding of its mechanisms and therapeutic potential.
Peer-Reviewed Studies on CO₂ Cryotherapy and Blood Flow
Recent peer-reviewed research has documented significant vascular effects of CO₂ cryotherapy across various clinical conditions and populations. Studies have investigated the effect of cryotherapy with carbon dioxide hydrate on fatigue recovery of neuromuscular function and muscle blood circulation, providing objective evidence of improved perfusion following treatment. Research methodologies include Doppler ultrasound measurements, laser Doppler flowmetry, and near-infrared spectroscopy to quantify blood flow changes. Studies consistently demonstrate immediate vasoconstriction followed by sustained vasodilation that exceeds baseline values. The magnitude and duration of vascular responses correlate with treatment parameters, including temperature, duration, and application frequency. Long-term studies show cumulative benefits with repeated applications, supporting the use of CO₂ cryotherapy in chronic condition management.
Infrared Thermography and Doppler Imaging Results
Advanced imaging techniques provide objective documentation of CO₂ cryotherapy’s vascular effects through real-time visualization of blood flow and temperature changes. Infrared thermography reveals immediate surface temperature reductions during application, followed by rebound warming that indicates enhanced circulation. Doppler imaging demonstrates quantifiable changes in vessel diameter, flow velocity, and perfusion patterns in response to treatment. Color Doppler studies show increased flow signals in treated areas during the vasodilation phase, confirming enhanced circulation. These imaging modalities allow practitioners to optimize treatment parameters and monitor individual patient responses. The objective nature of these measurements supports evidence-based treatment protocols and quality assurance in clinical practice.
Expert Opinions from Vascular Surgeons and Sports Physicians
Clinical experts from vascular surgery and sports medicine provide valuable insights into CO₂ cryotherapy’s practical applications and therapeutic potential. Vascular surgeons report improved outcomes when CO₂ cryotherapy is integrated into treatment protocols for circulation disorders and wound healing. Sports physicians document enhanced recovery rates and reduced injury recurrence in athletes receiving regular treatments. Expert consensus supports the use of CO₂ cryotherapy as an adjunctive therapy that complements traditional treatment approaches. Professional organizations are developing guidelines for optimal application protocols and safety procedures. The growing acceptance among medical specialists reflects the accumulating evidence supporting CO₂ cryotherapy’s safety and effectiveness in diverse clinical settings.

CO₂ 냉동 요법의 혜택은 누가 받을 수 있나요?
The broad applicability of CO₂ cryotherapy makes it suitable for diverse populations seeking improved circulation, pain relief, and enhanced recovery. Understanding the specific benefits for different groups helps optimize treatment approaches and outcomes.
운동선수 및 활동적인 개인
Athletes and physically active individuals represent the primary beneficiaries of CO₂ cryotherapy’s performance and recovery benefits. The enhanced circulation supports faster removal of metabolic waste products that contribute to muscle fatigue and delayed onset muscle soreness. Improved tissue oxygenation accelerates protein synthesis and cellular repair processes necessary for adaptation to training stress. The rapid pain relief allows continuation of training schedules with reduced discomfort and improved performance quality. Professional athletes report decreased recovery time between training sessions and competitions, enabling higher training volumes and intensities. The portable nature of CO₂ systems allows treatment at training facilities, competition venues, and during travel, making it practical for competitive athletes’ demanding schedules.
Patients with Circulatory Impairments
Individuals with various circulatory impairments can benefit from CO₂ cryotherapy’s ability to stimulate vascular function and improve tissue perfusion. Patients with peripheral arterial disease experience improved walking tolerance and reduced claudication symptoms through enhanced collateral circulation. Those with chronic venous insufficiency benefit from reduced lower extremity edema and improved venous return. Diabetic patients with microvascular complications show improved tissue perfusion and reduced risk of ulceration. The controlled nature of CO₂ application allows safe treatment of patients with compromised circulation who might not tolerate other forms of cold therapy. Treatment protocols must be individualized based on the severity of circulatory impairment and concurrent medical conditions.
Individuals with Inflammatory or Autoimmune Conditions
Systematic meta-analysis showed that exposure to cryotherapy may reduce inflammation by reducing the level of proinflammatory factors and increasing anti-inflammatory factors. Patients with rheumatoid arthritis, fibromyalgia, and other inflammatory conditions benefit from CO₂ cryotherapy’s anti-inflammatory and analgesic effects. The reduced inflammatory mediator activity helps manage joint pain and stiffness while improving mobility and function. The enhanced circulation supports nutrient delivery to affected tissues and promotes healing processes. The drug-free nature of the treatment makes it particularly valuable for patients seeking alternatives to pharmaceutical interventions or those experiencing medication side effects. Regular treatments can provide sustained symptom relief and improved quality of life for individuals with chronic inflammatory conditions.
Aging Populations Seeking Vascular Rejuvenation
Older adults seeking to maintain vascular health and combat age-related circulation decline can benefit from CO₂ cryotherapy’s rejuvenating effects. The enhanced endothelial function and improved nitric oxide production help maintain vascular flexibility and responsiveness. Regular treatments can slow the progression of age-related vascular changes and improve overall cardiovascular health. The skin rejuvenation effects provide cosmetic benefits while supporting healthy aging processes. The safety profile makes it suitable for older adults who may have multiple health conditions or take various medications. Treatment protocols can be adapted to accommodate reduced physiological reserve while maintaining therapeutic effectiveness. The non-invasive nature eliminates risks associated with more aggressive interventions.
Safety, Contraindications, and Best Practices
CO₂ 냉동 요법 is generally safe when administered by trained professionals following protocol. Its rapid cooling and short exposure time (10–15 seconds) prevent tissue damage, unlike more extreme cold therapies like liquid nitrogen. Safety features such as temperature control and automatic shut-off add further protection. Contraindications include severe peripheral vascular disease, Raynaud’s, cold urticaria, impaired sensation, or active infections. Pregnant women should avoid abdominal or lower back treatments. A thorough patient assessment is crucial. Best practices include pre-treatment screening, technique training, and post-treatment monitoring. Skin should be clean and dry; treatment requires steady, overlapping motion at the correct distance. Follow-up ensures results and adjustments as needed.
The Circulatory Power of Seconds: A Recap
CO₂ cryotherapy delivers powerful circulatory benefits in seconds through rapid vasoconstriction followed by enhanced vasodilation. This boosts blood flow, reduces inflammation, and stimulates tissue repair. Its effects extend beyond the session via cellular and neurovascular pathways. Clinically, it’s effective in sports recovery, pain relief, skin health, and vascular rehabilitation. Compared to traditional methods, its fast, targeted mechanism offers a modern, non-invasive solution with strong safety and growing evidence. As research expands, CO₂ cryotherapy is poised to play a larger role in circulation optimization and integrated care for diverse patient needs. Its ease of use and accessibility make it suitable for both clinical and at-home settings.
자주 묻는 질문(FAQ)
CO₂ cryotherapy delivers circulatory effects within 10–15 seconds. The rapid cooling triggers instant vasoconstriction, followed by rebound vasodilation that boosts blood flow. Patients often feel relief and warmth within the first minute, with benefits lasting up to 60 minutes. With repeated sessions, long-term vascular conditioning can develop.
The vascular response is both immediate and cumulative. Each session improves circulation for 30–90 minutes, while regular treatments enhance endothelial function, nitric oxide production, and capillary density. For lasting benefits, 2–3 sessions per week over 4–6 weeks are typically recommended.
It may help poor circulation by enhancing vasodilation, but for Raynaud’s, caution is essential. CO₂ cryotherapy can worsen symptoms in cold-sensitive individuals. Medical supervision and protocol adjustments are necessary to ensure safety and effectiveness.
Most users report a brief, intense cold sensation that fades quickly. The 10–15 second duration limits discomfort, and many feel immediate relief afterward. As circulation rebounds, warmth returns. Overall, the treatment is well-tolerated with minimal pain.
Rebound vasodilation stems from increased nitric oxide, reduced sympathetic tone, and vessel wall stimulation. These mechanisms override vasoconstriction, boosting blood flow and tissue oxygenation beyond baseline. The result is rapid, enhanced circulation in treated areas.
CO₂ cryotherapy offers targeted vascular stimulation—ideal for localized conditions. Whole-body cryo creates systemic effects but lacks precision. CO₂ is more convenient, cost-effective, and efficient for specific circulatory issues, while whole-body therapy suits general wellness needs.