Introduction: A Precision Cold Approach to Joint Dysfunction
Joint pain and stiffness affect millions worldwide, from athletes to aging adults. Traditional treatments often rely on drugs or invasive procedures, offering limited relief. CO₂ cryotherapy introduces a breakthrough: targeted cold therapy that addresses joint dysfunction at its source. Using pressurized carbon dioxide, this technique delivers rapid, localized cooling down to –78°C. Unlike general ice packs, it triggers immediate physiological responses—interrupting pain signals, reducing inflammation, and promoting healing. Its precision allows clinicians to apply cold exactly where needed, maximizing effectiveness while minimizing discomfort. Scientific research supports its multi-pathway benefits—from modulating inflammatory mediators to altering nerve conduction—making it a powerful, drug-free solution for joint pain that outperforms many conventional therapies.
The Biophysiology of Joint Stiffness and Pain
Understanding how CO₂ cryotherapy provides relief requires first examining the complex mechanisms underlying joint dysfunction. Joint pain and stiffness arise from intricate interactions between mechanical, inflammatory, and neurological processes that can create self-perpetuating cycles of discomfort and limited mobility.
Mechanical Contributors to Joint Dysfunction
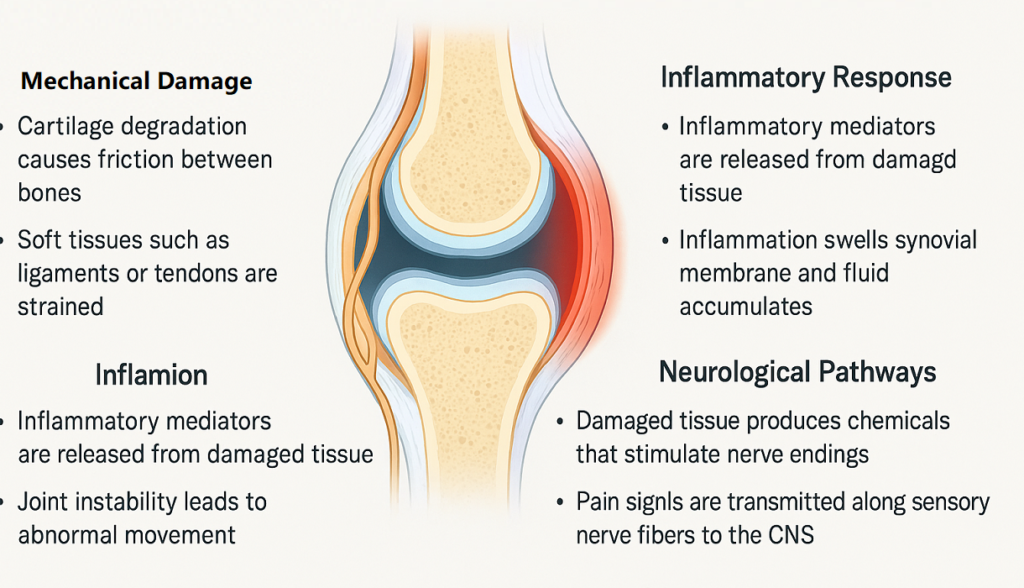
Joint stiffness often results from changes in the biomechanical integrity of periarticular tissues. Factors such as cartilage degradation, synovial fluid thickening, and capsular fibrosis restrict normal movement. Inflammatory conditions impair synovial production of hyaluronic acid, increasing joint surface friction and accelerating wear. Additionally, protective muscle guarding around painful joints causes involuntary contractions that limit range of motion and elevate joint stress. These compensatory mechanisms, though protective, lead to inefficiency in joint function and reinforce the pain-stiffness cycle. Chronic inflammation can also induce capsular and ligamentous contractures through fibrosis and collagen cross-linking. These structural adaptations permanently alter joint motion and shift mechanical loads to surrounding tissues, creating dysfunction in adjacent joints and compounding the overall problem.
Inflammatory and Neurological Pathways of Pain
Joint inflammation involves a complex cascade of cytokines and immune responses. Key mediators like IL-1β, IL-6, and TNF-α increase vascular permeability, recruit immune cells, and activate nociceptors. These cytokines also trigger prostaglandin and leukotriene production, directly heightening pain sensitivity. Localized cooling, such as applying ice to arthritic knees, has demonstrated the ability to reduce intra-articular temperatures and suppress inflammatory activity, inducing a temporary anti-inflammatory state. Neurologically, both nociceptive and neuropathic elements contribute to pain. A-delta and C-fiber nociceptors within joints respond to mechanical and chemical triggers. With ongoing stimulation, central sensitization develops—heightening spinal neuron excitability and resulting in symptoms like allodynia and hyperalgesia typical of chronic joint pain.
Conventional Therapies and Their Therapeutic Gaps
Conventional joint pain treatments include NSAIDs, corticosteroids, viscosupplementation, and physical therapy. While NSAIDs are effective short-term, long-term use increases risks of GI bleeding, cardiovascular events, and renal impairment. Corticosteroid injections can relieve acute symptoms but may damage cartilage with repeated use. Hyaluronic acid injections offer mixed results and require multiple treatments. Physical therapy improves mobility over time but often lacks immediate impact. These therapies target symptoms rather than root causes and may not address inflammation, nerve sensitization, and biomechanical issues simultaneously. As a result, patients often require complex, combined approaches that increase treatment burden and risk of side effects. CO₂ cryotherapy offers an innovative, non-invasive alternative with the potential to deliver rapid, multi-mechanism relief while minimizing systemic exposure.
CO₂ Cryotherapy: The Science Behind the Soothe
The therapeutic efficacy of CO₂ cryotherapy lies in its unique ability to deliver precise, controlled cooling that triggers multiple beneficial physiological responses. Understanding the scientific principles underlying this technology reveals why it offers superior outcomes compared to traditional cold therapy approaches.
The Physics of CO₂ Cooling
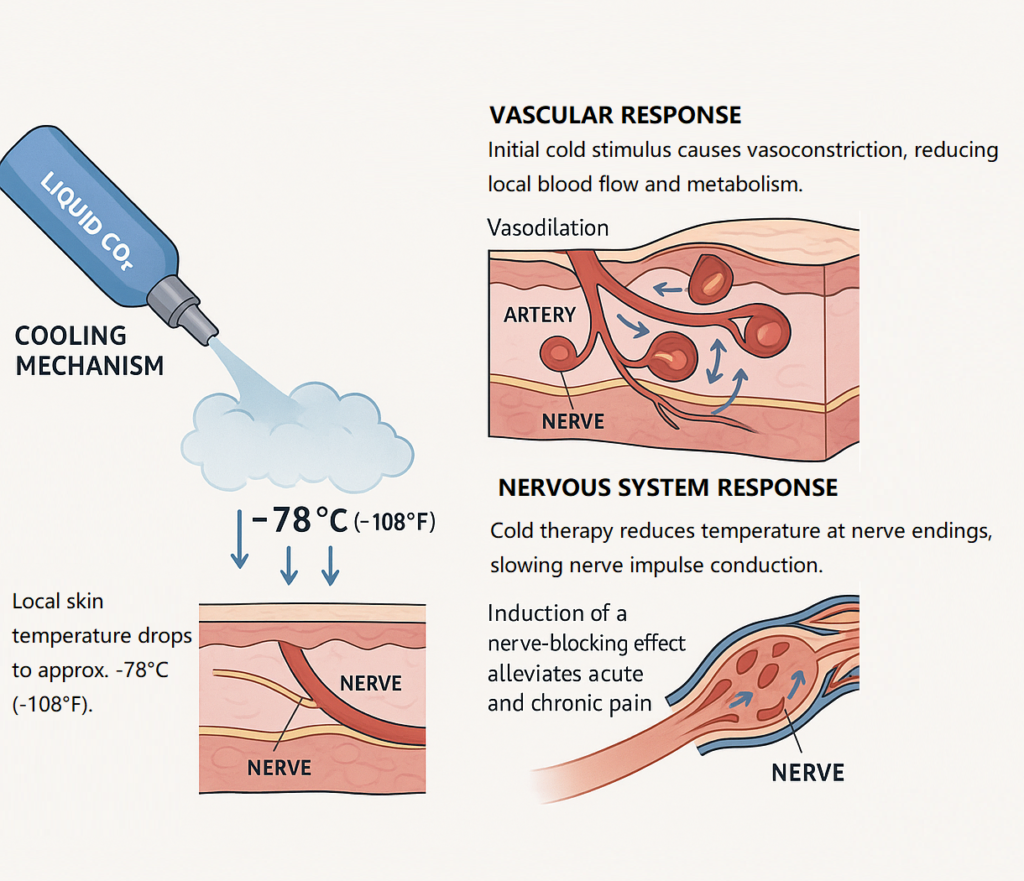
CO₂ cryotherapy works through the rapid phase transition of pressurized liquid CO₂ into gas upon release. As CO₂ expands, it produces a dry snow-like stream that reaches –78°C at the application site. This cooling process follows the Joule-Thomson effect, where gas expansion causes significant temperature drops without needing external energy. The treatment uses three cooling mechanisms: conduction (initial skin cooling), convection (cold gas flow around the area), and sublimation (CO₂ snow turning to gas, absorbing heat). These mechanisms work together to create rapid, controlled, and deep-penetrating cooling—far more efficient than standard ice packs. Clinicians can fine-tune the intensity and duration based on joint condition and patient tolerance, delivering precise therapeutic cold for maximum impact with minimal discomfort.
Vascular and Neuromuscular Effects on Joint Environment
CO₂ cryotherapy triggers immediate vasoconstriction via alpha-adrenergic receptor activation, reducing blood flow and limiting inflammation. After initial constriction, reactive vasodilation improves circulation, enhances oxygenation, and supports tissue repair. On a neuromuscular level, lower skin temperatures slow nerve conduction, creating a temporary numbing effect that interrupts pain signaling. Motor neuron activity also decreases, reducing muscle spasm and guarding. This cold exposure impacts cellular metabolism, lowering enzymatic breakdown of cartilage and suppressing inflammation-producing compounds. The joint capsule and synovium benefit from reduced metabolic stress, while controlled hypothermia preserves cellular integrity and promotes recovery—making it effective not only for pain relief but also for tissue protection.
Why CO₂ Outperforms Traditional Cold Applications
CO₂ cryotherapy offers precise, localized treatment unmatched by ice packs or whole-body cryo. Clinicians can target affected joints without cooling nearby healthy tissue, enhancing results while minimizing discomfort. Sessions last just 10–15 seconds per site, compared to 15–20 minutes with traditional methods. The dry, controlled application reduces risks like frostbite or prolonged tissue numbness. Unlike ice packs, which cool inconsistently, CO₂ systems provide consistent, calibrated thermal doses, allowing for evidence-based protocols and predictable outcomes. Treatment can be adjusted in real time to match patient sensitivity and joint type. For busy clinics or patients needing fast recovery, CO₂ cryotherapy delivers efficiency, accuracy, and reproducible therapeutic results.
Therapeutic Impact: How the Cold Translates to Comfort
The clinical benefits of CO₂ cryotherapy extend beyond simple pain relief, encompassing improvements in joint function, mobility, and overall quality of life. Understanding these therapeutic impacts helps explain why CO₂ cryotherapy has gained recognition as an effective treatment modality for various joint conditions.
Measurable Improvements in Joint Functionality
CO₂ cryotherapy leads to measurable gains in joint function. Studies show immediate increases in both active and passive range of motion, with goniometric improvements averaging 10–15° across various joints. These effects can last for hours post-treatment. Dynamometry reveals reduced pain-related inhibition, allowing patients to produce more force during muscle testing without discomfort. This correlates with improved performance in daily activities. Pressure-sensitive gait and joint loading analyses show more symmetrical movement, better balance, and reduced compensatory stress post-treatment. These findings suggest CO₂ cryotherapy not only relieves symptoms but also improves joint mechanics and movement quality—addressing underlying dysfunction patterns, not just surface-level pain.
Patient-Reported Outcomes and Recovery Experience
Patients report fast and lasting relief following CO₂ cryotherapy. Pain often decreases 30–50% within minutes, with effects lasting 2–4 hours or longer after one session. Validated outcome scores like WOMAC and DASH improve after treatment cycles, with patients noting easier movement during work, daily routines, and recreation. Many also report better sleep due to reduced nighttime pain and a notable drop in medication reliance—helping avoid side effects from chronic painkillers. CO₂ cryotherapy is consistently rated as comfortable, fast-acting, and easy to integrate into recovery routines, improving overall quality of life and satisfaction with joint care.
Expert Use in Clinical and Sports Medicine
CO₂ cryotherapy is widely adopted in sports and rehab settings. In athletics, it’s used pre-game to enhance joint mobility and post-game to reduce DOMS and speed up recovery. Orthopedic specialists apply it to manage osteoarthritis, tendinopathies, and post-op inflammation. Its precision allows safe use alongside other therapies. Physical therapists often use CO₂ cryotherapy before rehab exercises to reduce pain, helping patients participate more actively in training sessions. This strategy improves compliance, accelerates functional recovery, and supports better long-term outcomes—making it a versatile tool in both prevention and rehabilitation protocols.

Application Guidelines: Personalized Use of CO₂ Cryo
Effective CO₂ cryotherapy requires careful consideration of patient selection, treatment parameters, and individualized protocols. Proper application guidelines ensure optimal therapeutic outcomes while maintaining safety standards across diverse patient populations.
Indications: Who Needs CO₂ Cryotherapy Most
CO₂ cryotherapy is especially effective for acute inflammatory joint conditions like post-traumatic arthritis, osteoarthritis flare-ups, and autoimmune arthropathies. Its rapid anti-inflammatory action provides quick symptom relief and improves joint function. Chronic musculoskeletal issues—such as degenerative joint disease and tendinopathies—also respond well. By breaking the pain-spasm cycle, CO₂ therapy allows better participation in physical rehabilitation. Athletes with acute sprains, strains, or contusions benefit from localized cooling, which helps limit inflammation while supporting healing. It’s commonly used by both elite and recreational athletes not only for injury recovery, but also as a tool to optimize performance and reduce delayed onset muscle soreness (DOMS) after training.
Anatomical Target Zones and Delivery Protocols
Knee treatments target joint lines, suprapatellar pouch, and posterior capsule. Most protocols include 3–4 application sites per knee, each exposed to CO₂ for 10–15 seconds. Applicators are held 2–3 cm from the skin for safe, even cooling. For shoulder joints, cooling is applied to the anterior/posterior capsules, AC joint, and rotator cuff insertions. Due to its complexity, multiple angles may be used to access relevant structures fully. Spine-focused treatments address facet joints, SI joints, and myofascial trigger points. Since nerves are nearby, clinicians use shorter exposure times and greater distances for safety. Each anatomical site requires tailored cooling strategies to maximize therapeutic effects without risking skin or nerve injury.
Treatment Planning and Frequency Models
A typical treatment series begins with 3–5 sessions over 1–2 weeks. Each session is spaced 48–72 hours apart to allow tissue recovery and guide adjustments. Clinicians monitor early responses to refine dosing and application zones. Maintenance schedules vary. Chronic pain may benefit from weekly treatments, while acute flares may only need as-needed care. Some patients receive sessions before high-risk activities to prevent recurrence. Frequency also depends on age, circulation, medication, and training demands. Older or medically complex patients may need extended recovery time, while athletes in peak training cycles can tolerate more frequent use. Personalized scheduling ensures safety while maintaining therapeutic momentum.
Safety Profile, Contraindications, and Clinical Oversight
While CO₂ cryotherapy demonstrates an excellent safety profile when properly administered, understanding potential risks and contraindications ensures safe clinical practice and optimal patient outcomes.
Risk Management in Cryo Application
The main safety goal of CO₂ cryotherapy is to prevent cold-related injury through proper technique and real-time monitoring. Skin temperature should be tracked during sessions to avoid frostbite or burns; modern systems offer built-in temperature sensors and automatic shutoffs for added protection. To prevent localized tissue damage, clinicians use a continuous “painting” technique—moving the applicator evenly across the target area for 10–15 seconds per site. Clear communication ensures patients report discomfort promptly. They should be educated on what sensations are expected (cold, tingling) versus concerning (numbness, burning). All clinics should establish emergency protocols to handle adverse reactions quickly and safely. With proper training and patient feedback, CO₂ cryotherapy maintains a strong safety profile across treatment settings.
Patient Profiles Requiring Caution
Certain patient groups require extra care when using CO₂ cryotherapy. Those with peripheral vascular disease may have impaired circulation, increasing the risk of cold injury. Diabetic patients with neuropathy may not feel temperature extremes, so monitoring and protocol adjustments are essential. Conditions like Raynaud’s phenomenon, cold urticaria, and cryoglobulinemia can trigger abnormal cold responses and should be screened for. Test spots may help assess tolerance before proceeding with full treatment. Pregnancy is a general exclusion due to limited data on fetal response to localized cold exposure. Pediatric patients require shorter durations and careful supervision, as they cool more quickly than adults. Individualized protocols help ensure safety while preserving treatment benefits.
Conclusion: A Cool Solution for Hot Joints
CO₂ cryotherapy offers a major step forward in non-drug joint pain management, delivering precise cooling that targets inflammation, neuromuscular tension, and impaired mobility. Its strong safety profile, rapid results, and patient-friendly application make it ideal for both acute and chronic joint issues. By relieving pain and enhancing joint function, CO₂ cryotherapy supports long-term recovery and fits well into personalized, low-risk treatment plans. As demand grows for effective, side effect–free therapies, this technology meets modern clinical and patient expectations. Future advances will likely enhance precision, monitoring, and treatment flexibility. Ongoing studies will help fine-tune protocols and explore combined therapies for even better results. Integrating CO₂ cryotherapy into routine care empowers clinicians to reduce medication use and deliver better outcomes—making it a smart, forward-looking choice in comprehensive joint care.
FAQs
CO₂ cryotherapy uses carbon dioxide gas to deliver precise, controlled cold temperatures to affected joints. Unlike ice packs, it provides rapid cooling with consistent temperature control, minimizing tissue damage and enhancing therapeutic effects.
The cold causes vasoconstriction followed by reactive vasodilation, improves blood flow, reduces inflammation, and modulates nerve signaling to decrease pain and improve joint mobility.
Patients with chronic joint stiffness, osteoarthritis, sports injuries, or inflammatory joint conditions can benefit, especially when conventional therapies have not provided sufficient relief.
When properly administered, CO₂ cryotherapy has an excellent safety profile suitable for regular use. Treatment frequency depends on individual conditions and response patterns, typically ranging from weekly maintenance to as-needed applications.
While generally safe, CO₂ cryotherapy should be avoided or carefully managed in patients with cold hypersensitivity, circulatory issues, open wounds, or certain neurological conditions. Proper clinical oversight is essential.
Treatment plans vary but often involve multiple sessions (e.g., weekly treatments) over several weeks. Clinical response depends on the severity and type of joint dysfunction.
Yes, it is often used as part of a multimodal approach including physical therapy, medication, or injections to maximize joint function and pain relief.



