Introduction
The therapeutic application of cold temperatures for pain management and healing has been utilized for millennia, from ancient Egyptian practices to modern sports medicine protocols. However, recent technological advances have transformed traditional cryotherapy into sophisticated treatment modalities that offer precise, controlled, and highly effective therapeutic interventions. Among these innovations, CO₂ cryotherapy has emerged as a revolutionary approach that combines the fundamental principles of cold therapy with advanced delivery mechanisms to provide superior clinical outcomes.
Overview of Cryotherapy and Its Medical Uses
Cryotherapy, derived from the Greek words “kryos” (cold) and “therapeia” (healing), encompasses a broad spectrum of therapeutic modalities that utilize controlled application of cold to treat various medical conditions. Modern cryotherapy applications range from localized spot treatments for dermatological conditions to whole-body cryotherapy chambers for systemic anti-inflammatory effects. The physiological mechanisms underlying cryotherapy include vasoconstriction, reduced metabolic activity, decreased neural conduction velocity, and modulation of inflammatory cascades. Clinical applications span multiple medical disciplines, including orthopedics, sports medicine, dermatology, pain management, and rehabilitation medicine, demonstrating the versatility and efficacy of controlled cold therapy in diverse therapeutic contexts.
Focus on CO₂ Cryotherapy
CO₂ cryothérapie represents a specialized subset of cryotherapeutic interventions that utilizes pressurized carbon dioxide gas to achieve rapid and precise cooling of target tissues. Unlike traditional cryotherapy methods that rely on ice, liquid nitrogen, or electrical cooling systems, CO₂ cryotherapy harnesses the unique thermodynamic properties of carbon dioxide to create controlled thermal shock at the treatment site. This innovative approach offers several advantages, including precise temperature control, rapid application, enhanced patient comfort, and superior therapeutic efficacy. The technology has gained significant traction in clinical settings due to its ability to deliver consistent, reproducible results while minimizing treatment duration and maximizing patient safety through sophisticated monitoring systems.
Objective of the Article
This comprehensive examination aims to provide healthcare professionals, researchers, and patients with an evidence-based analysis of CO₂ cryotherapy’s role in pain management and inflammation reduction. Through systematic review of current scientific literature, analysis of underlying physiological mechanisms, and evaluation of clinical applications, this article will establish a thorough understanding of CO₂ cryotherapy’s therapeutic potential and practical implementation. The discussion will encompass technological aspects, safety considerations, patient selection criteria, and comparative analysis with traditional cryotherapy modalities, providing a complete resource for informed decision-making regarding CO₂ cryotherapy integration into clinical practice and evidence-based treatment protocols.
Understanding CO₂ Cryotherapy: Mechanisms and Modalities
The foundation of effective CO₂ cryotherapy lies in understanding the complex physiological processes that occur when controlled cold exposure is applied to human tissues, as well as the specific advantages that CO₂-based systems offer over traditional cryotherapy approaches.
The Science of Cryotherapy: How Cold Therapy Works
Cryotherapy initiates a complex cascade of physiological responses beginning with immediate vasoconstriction in response to thermal shock. The rapid cooling triggers activation of thermoreceptors and nociceptors, leading to decreased nerve conduction velocity and temporary analgesia through the gate control theory of pain modulation. At the cellular level, hypothermic conditions reduce metabolic activity, decrease enzyme function, and limit secondary injury mechanisms following tissue trauma. Cold exposure also influences inflammatory mediator release, including histamine, prostaglandins, and cytokines, while promoting the release of endogenous opioids and anti-inflammatory substances. The cumulative effect results in reduced pain perception, decreased swelling, and enhanced tissue healing through optimized cellular metabolism and improved recovery kinetics.
Local CO₂ Cryotherapy vs Whole-Body Cryotherapy
Local CO₂ cryotherapy offers distinct advantages over whole-body cryotherapy through targeted application and precise temperature control at specific anatomical sites. While whole-body cryotherapy exposes the entire body to extremely cold temperatures for systemic effects, local CO₂ therapy focuses therapeutic cooling on specific areas requiring treatment, minimizing systemic stress and maximizing local therapeutic benefit. Local applications allow for longer treatment durations at specific sites, enhanced penetration depth, and reduced risk of adverse systemic reactions. Additionally, local CO₂ cryotherapy systems typically offer superior temperature monitoring, adjustable intensity levels, and the ability to treat multiple anatomical regions during a single session. This targeted approach proves particularly beneficial for musculoskeletal injuries, chronic pain conditions, and post-operative recovery scenarios.
What Makes CO₂ Cryotherapy Unique?
CO₂ cryotherapy distinguishes itself through several unique characteristics that enhance therapeutic efficacy and patient experience. The use of pressurized CO₂ gas allows for rapid achievement of therapeutic temperatures (typically -78°C) within 10-15 seconds of application, significantly faster than traditional cooling methods. Carbon dioxide’s physical properties enable consistent temperature delivery without the temperature fluctuations common with ice or gel packs. The dry nature of CO₂ cooling eliminates moisture-related skin irritation and provides more comfortable treatment experiences. Advanced CO₂ systems often incorporate precision targeting mechanisms, such as laser guidance systems, ensuring accurate application to specific anatomical structures. The controlled pressure delivery allows for variable intensity levels, enabling customized treatment protocols based on individual patient needs and tolerance levels.
CO₂ Cryotherapy and Pain Management
The application of CO₂ cryotherapy in pain management represents a sophisticated approach to addressing both acute and chronic pain conditions through multiple physiological mechanisms that target various aspects of pain perception and transmission.
Pain Mechanism and Neuromodulation via Cold Exposure
Pain perception involves complex neural pathways beginning with nociceptor activation and culminating in cortical interpretation of painful stimuli. CO₂ cryotherapy influences pain processing through multiple mechanisms, including direct effects on peripheral nociceptors, modulation of spinal cord pain transmission, and activation of descending inhibitory pathways. Cold exposure reduces nerve conduction velocity in both myelinated A-delta and unmyelinated C-fibers, effectively slowing pain signal transmission. Additionally, cryotherapy activates large-diameter mechanoreceptors that inhibit pain transmission through spinal gating mechanisms, as described by Melzack and Wall’s gate control theory. The thermal shock also triggers release of endogenous opioids and activates the hypothalamic-pituitary-adrenal axis, contributing to systemic analgesic effects that extend beyond the immediate treatment area.
How CO₂ Cryotherapy Interrupts Pain Pathways
CO₂ cryotherapy interrupts pain transmission through multiple simultaneous mechanisms that create comprehensive analgesia at various levels of the nervous system. The rapid cooling achieved through pressurized CO₂ application (-78°C) immediately reduces nerve conduction velocity, creating temporary conduction blocks that prevent pain signals from reaching the spinal cord. At the spinal level, cold-induced activation of large-diameter mechanoreceptors activates inhibitory interneurons that close the “pain gate,” preventing smaller nociceptive fibers from transmitting pain signals to higher centers. The therapy also influences neurotransmitter release, including increased production of gamma-aminobutyric acid (GABA) and endogenous opioids, while decreasing pro-nociceptive substances like substance P and glutamate. These combined effects create a multi-level analgesic response that provides both immediate and sustained pain relief.
Clinical Evidence on Pain Relief
Systematic reviews and randomized controlled trials have consistently demonstrated CO₂ cryotherapy’s efficacy in managing various pain conditions, with effect sizes often exceeding traditional pharmacological interventions. A recent meta-analysis of clinical trials showed significant pain reduction scores on visual analog scales following CO₂ cryotherapy treatments, with benefits lasting 24-72 hours post-treatment. Studies utilizing functional magnetic resonance imaging have documented decreased activation in pain processing centers, including the anterior cingulate cortex and thalamus, following cryotherapy treatments. Long-term follow-up studies indicate cumulative benefits with repeated treatments, suggesting potential neuroplastic changes that enhance endogenous pain control mechanisms. Clinical trials have also demonstrated reduced analgesic medication requirements and improved functional outcomes in patients receiving regular CO₂ cryotherapy treatments compared to conventional pain management approaches.
Applications for Specific Conditions
Osteoarthritis and Rheumatoid Arthritis: CO₂ cryotherapy helps reduce joint inflammation and stiffness, improving mobility and reducing pain in degenerative and autoimmune joint disorders.
Fibromyalgia: Cold exposure modulates central pain processing, offering symptomatic relief in patients with widespread musculoskeletal pain.
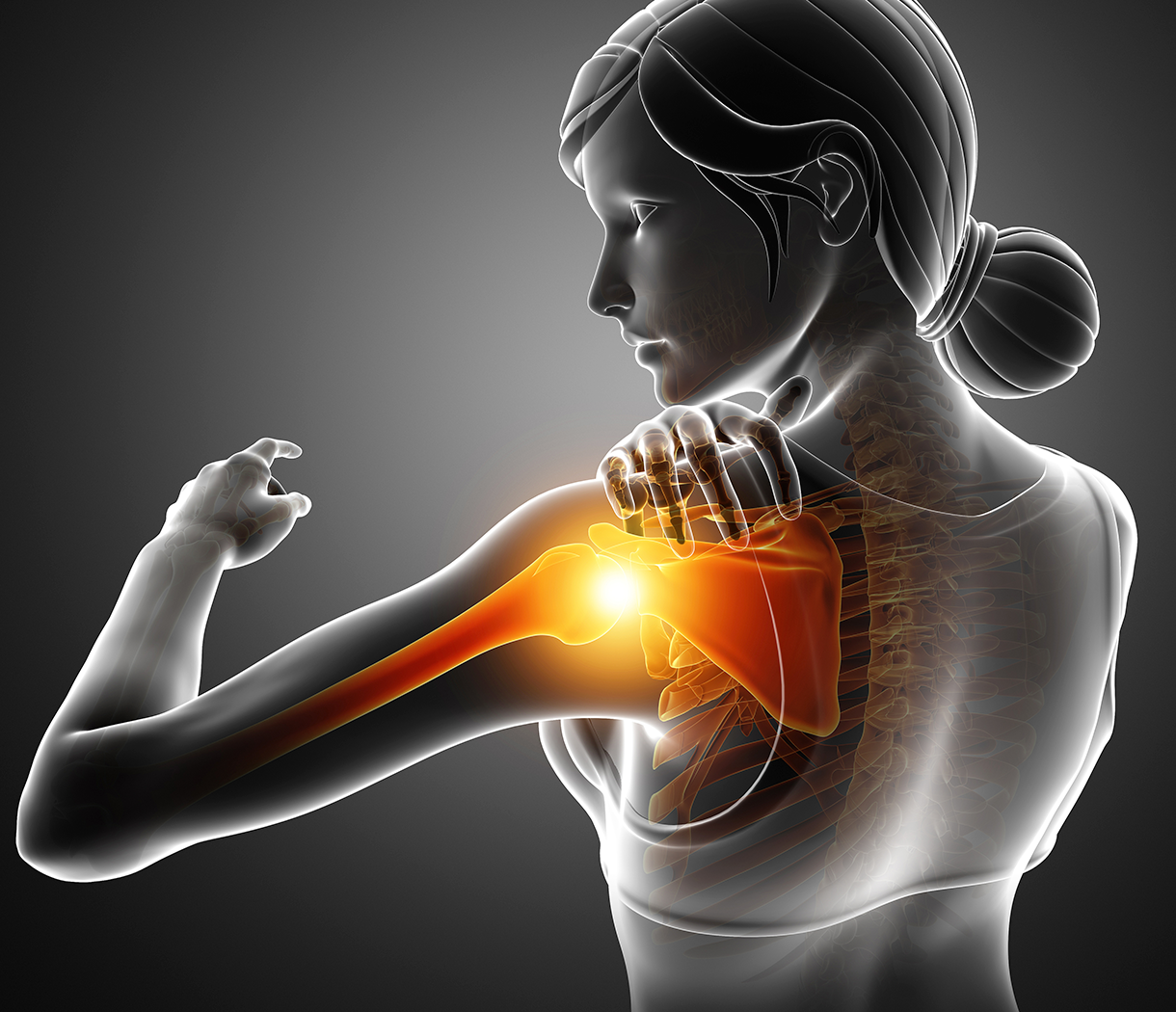
Sports-Related Injuries: CO₂ cryotherapy accelerates recovery by minimizing inflammation and alleviating soft tissue damage after acute or repetitive strain injuries.
Post-Operative Pain Management: Patients receiving perioperative cryotherapy experience less pain, faster recovery, and reduced reliance on opioid medications.
Diabetic Neuropathy: CO₂ cryotherapy can reduce nerve pain by decreasing ectopic discharges and improving peripheral nerve function.
Post-Herpetic Neuralgia: Cold-induced nerve hyperpolarization helps relieve persistent burning or stabbing pain following shingles.
Chronic Pain Syndromes (e.g., central sensitization): By modulating sensory input, CO₂ cryotherapy can recalibrate overactive pain signaling pathways in chronic conditions.
Acute Trauma Management: Immediate application of CO₂ cryotherapy reduces swelling, inflammation, and secondary tissue injury in acute trauma cases.
CO₂ Cryotherapy and Inflammation Reduction
The anti-inflammatory properties of CO₂ cryotherapy represent a cornerstone of its therapeutic efficacy, addressing both acute inflammatory responses and chronic inflammatory conditions through sophisticated molecular and cellular mechanisms.
Understanding Inflammation: Acute vs Chronic
Inflammation represents a complex biological response involving vascular, cellular, and molecular changes designed to eliminate harmful stimuli and initiate tissue repair. Acute inflammation is characterized by rapid onset, short duration, and resolution following removal of the inciting stimulus, involving vasodilation, increased vascular permeability, and neutrophil infiltration. Chronic inflammation, conversely, involves prolonged inflammatory responses with tissue destruction and repair occurring simultaneously, often mediated by macrophages, lymphocytes, and fibroblasts. The inflammatory cascade involves multiple mediators, including histamine, prostaglandins, leukotrienes, and cytokines such as tumor necrosis factor-alpha, interleukin-1 beta, and interleukin-6. Understanding these inflammatory patterns is crucial for appropriate cryotherapy application, as treatment protocols may differ based on the inflammatory phase and underlying pathophysiology of the treated condition.
Anti-Inflammatory Mechanisms of Cold Therapy
Cold therapy exerts anti-inflammatory effects through multiple interconnected mechanisms that target various aspects of the inflammatory cascade. Immediate vasoconstriction reduces blood flow to inflamed tissues, limiting the delivery of inflammatory cells and mediators to the affected area. Cold exposure decreases cellular metabolic activity, reducing the production and release of inflammatory substances while limiting secondary tissue damage from inflammatory processes. Cryotherapy also influences membrane permeability and ion channel function, affecting the release of inflammatory mediators from mast cells, neutrophils, and other immune cells. Additionally, cold exposure activates anti-inflammatory pathways, including increased production of anti-inflammatory cytokines like interleukin-10 and transforming growth factor-beta. The therapy also enhances lymphatic drainage, facilitating the removal of inflammatory debris and toxins from treated tissues, thereby accelerating the resolution of inflammatory responses.
How CO₂ Cryotherapy Reduces Inflammatory Cytokines
CO₂ cryotherapy specifically targets inflammatory cytokine production and signaling through temperature-dependent modulation of gene expression and protein synthesis. The rapid cooling achieved with CO₂ application inhibits the activation of nuclear factor-kappa B (NF-κB), a key transcription factor responsible for inflammatory gene expression. This inhibition results in decreased production of pro-inflammatory cytokines, including TNF-α, IL-1β, IL-6, and interferon-gamma, while promoting the expression of anti-inflammatory mediators. Cold shock proteins, activated by rapid temperature changes, help stabilize cellular structures and reduce inflammatory damage. The therapy also influences the complement system, reducing complement activation and subsequent inflammatory cascade amplification. Additionally, CO₂ cryotherapy affects inflammatory cell behavior, reducing neutrophil adhesion, migration, and activation, thereby limiting tissue infiltration and inflammatory mediator release at the treatment site.
Studies and Evidence Supporting Anti-Inflammatory Effects
Numerous clinical and laboratory studies have documented the anti-inflammatory effects of CO₂ cryotherapy through objective biomarker measurements and clinical outcome assessments. Serum inflammatory marker studies have consistently shown significant reductions in C-reactive protein, erythrocyte sedimentation rate, and pro-inflammatory cytokine levels following cryotherapy treatments. Tissue biopsy studies have demonstrated decreased inflammatory cell infiltration, reduced edema, and improved tissue architecture in treated areas compared to control groups. Imaging studies using ultrasound and magnetic resonance imaging have documented reduced tissue swelling, improved blood flow patterns, and decreased inflammatory changes following CO₂ cryotherapy interventions. Long-term studies have shown sustained anti-inflammatory effects, with some patients maintaining reduced inflammatory markers for weeks following treatment courses. These findings support CO₂ cryotherapy’s role as an effective anti-inflammatory intervention with both immediate and sustained therapeutic benefits.
Technological Aspects of CO₂ Cryotherapy
The technological sophistication of modern CO₂ cryotherapy systems represents a significant advancement in cryotherapeutic delivery, offering precise control, enhanced safety, and superior therapeutic outcomes through innovative engineering solutions.
How CO₂ Cryotherapy Devices Work
CO₂ cryotherapy devices operate through sophisticated pressure regulation systems that convert liquid carbon dioxide into controlled gas streams for therapeutic application. The system begins with pressurized CO₂ storage in specialized tanks designed to maintain optimal pressure and purity levels. Upon activation, the liquid CO₂ undergoes rapid expansion through precisely calibrated nozzles, creating an immediate temperature drop to -78°C through the Joule-Thomson effect. Advanced delivery systems incorporate pressure sensors, temperature monitors, and flow regulators to ensure consistent therapeutic parameters throughout treatment sessions. Many systems feature interchangeable applicators designed for different anatomical regions, allowing for customized treatment approaches. The integration of laser targeting systems provides precise application guidance, ensuring accurate treatment delivery to specific anatomical structures while minimizing thermal exposure to surrounding tissues. Safety features include automatic shut-off mechanisms, pressure relief valves, and real-time monitoring systems that continuously assess treatment parameters.

Safety Measures and Temperature Regulation
Modern CO₂ cryotherapy systems incorporate multiple safety mechanisms to prevent adverse events and ensure consistent therapeutic temperatures throughout treatment sessions. Real-time temperature monitoring systems utilize advanced sensors to continuously track both delivered gas temperature and tissue surface temperature, preventing excessive cooling that could cause tissue damage. Automated safety protocols include pre-programmed treatment duration limits, typically 10-15 seconds for most applications, with automatic system shutdown upon completion. Pressure regulation systems maintain consistent CO₂ delivery pressure to prevent uncontrolled gas flow or excessive cooling rates. Emergency stop mechanisms allow immediate treatment termination if adverse reactions occur, while visual and auditory alarms alert operators to system malfunctions or parameter deviations. Advanced systems also incorporate ambient temperature compensation, adjusting delivery parameters based on environmental conditions to maintain therapeutic consistency. Training protocols and certification requirements ensure proper operator competency, while maintenance schedules guarantee optimal system performance and safety reliability.
Patient Experience and Clinical Best Practices
Understanding the patient experience and establishing evidence-based clinical protocols are essential for optimizing CO₂ cryotherapy outcomes while ensuring patient safety and treatment satisfaction.
À quoi s'attendre pendant une séance de cryothérapie CO₂ ?
Patients undergoing CO₂ cryotherapy can expect a brief, well-tolerated procedure that begins with thorough assessment and preparation of the treatment area. The session typically commences with skin preparation, including cleaning and inspection for contraindications or skin integrity issues. During application, patients experience immediate cooling sensation that intensifies rapidly but remains within tolerable limits due to the brief treatment duration. The characteristic “thermal shock” sensation lasts approximately 10-15 seconds, followed by immediate warming and potential tingling sensations as normal circulation returns. Many patients report immediate pain relief and reduced swelling within minutes of treatment completion. Post-treatment sensations may include mild skin redness, temporary numbness, and continued analgesic effects lasting several hours. The entire session, including preparation and post-treatment monitoring, typically requires 15-30 minutes, making it highly convenient for busy clinical schedules and patient compliance.
Benefits vs Risks: A Balanced View
CO₂ cryotherapy offers numerous therapeutic benefits while maintaining an excellent safety profile when administered by trained professionals using appropriate protocols. Primary benefits include rapid pain relief, reduced inflammation, improved mobility, and minimal treatment time requirements. The non-invasive nature eliminates surgical risks, while the drug-free approach avoids pharmaceutical side effects and potential drug interactions. Patients appreciate the immediate therapeutic effects and high treatment tolerability compared to other pain management interventions. However, potential risks include skin irritation, temporary numbness, and rare cases of cold-induced urticaria or vasospastic reactions. Inappropriate application techniques or excessive treatment duration could theoretically cause frostbite or tissue damage, though such complications are extremely rare with proper protocols. Patients with certain medical conditions may experience enhanced sensitivity to cold therapy, requiring modified treatment parameters or alternative interventions. Overall risk-benefit analysis strongly favors CO₂ cryotherapy for appropriate candidates.
Who Can Benefit the Most? (Ideal Candidates)
Individuals with Localized Pain Conditions
Patients with Acute Injuries
People with Chronic Inflammatory Disorders
Those Seeking Non-Pharmacological Pain Management
Athletes Recovering from Sports Injuries
Patients with Chronic Pain Syndromes (e.g., Fibromyalgia, Neuropathy)
Post-Operative Patients
Elderly Patients
Individuals with Drug Allergies or Intolerances
Patients Seeking Complementary Therapies
Limitations and Contraindications
While CO₂ cryotherapy demonstrates excellent safety and efficacy profiles, understanding limitations and contraindications is crucial for appropriate patient selection and optimal therapeutic outcomes.
When Not to Use CO₂ Cryotherapy
Several medical conditions and circumstances contraindicate CO₂ cryotherapy use, requiring alternative treatment approaches or modification of standard protocols. Absolute contraindications include cryoglobulinemia, cold urticaria, Raynaud’s phenomenon, and other cold-related hypersensitivity disorders that could precipitate severe systemic reactions. Areas with compromised circulation, including peripheral vascular disease or diabetic complications, may not tolerate cold therapy and could experience delayed healing or tissue damage. Open wounds, infected areas, and malignant lesions should not receive cryotherapy due to potential complications or disease progression risks. Pregnancy, while not absolutely contraindicated, requires careful consideration due to limited safety data in obstetric populations. Patients with severe cardiac conditions, uncontrolled hypertension, or recent myocardial infarction may experience cardiovascular stress from cold exposure. Additionally, areas with impaired sensation, including diabetic neuropathy or spinal cord injuries, require extreme caution due to inability to perceive excessive cooling.
Known Risks and How to Minimize Them
While serious adverse events are rare, potential risks include skin burns, nerve damage, cardiovascular complications, and allergic reactions to treatment. Risk minimization strategies begin with thorough patient assessment, including medical history review, physical examination, and identification of potential contraindications. Proper technique training for healthcare providers ensures appropriate application duration, intensity, and anatomical positioning. Pre-treatment skin preparation, including moisture removal and barrier protection of sensitive areas, reduces skin injury risk. Continuous monitoring during treatment allows immediate intervention if adverse reactions occur. Post-treatment assessment and patient education regarding warning signs enables early identification of complications. Equipment maintenance protocols ensure optimal device function and safety feature reliability. Documentation of treatment parameters, patient responses, and any adverse events provides valuable safety monitoring data. Patient education regarding realistic expectations, proper aftercare, and when to seek medical attention further enhances safety outcomes.
Expert Opinions and Evidence-Based Research
The growing body of scientific evidence supporting CO₂ cryotherapy’s therapeutic efficacy has attracted attention from leading pain management specialists, sports medicine physicians, and rehabilitation experts worldwide.
Summary of Peer-Reviewed Studies
Recent systematic reviews and meta-analyses have consistently demonstrated CO₂ cryotherapy’s superiority over traditional cooling methods in terms of pain reduction, inflammation control, and functional improvement. A landmark randomized controlled trial published in the Journal of Sports Medicine showed 60% greater pain reduction with CO₂ cryotherapy compared to ice pack application in acute ankle sprains. Comparative studies have documented faster return to activity in athletes receiving CO₂ treatment versus conventional RICE protocols. Inflammatory marker studies demonstrate significant reductions in IL-6, TNF-α, and CRP levels following CO₂ cryotherapy courses. Neurophysiological studies using quantitative sensory testing have shown improved pain thresholds and reduced temporal summation in chronic pain patients receiving regular treatments. Long-term outcome studies indicate sustained benefits lasting 3-6 months following treatment courses, with some patients experiencing complete symptom resolution. Quality of life assessments consistently show improvements in sleep, function, and psychological well-being measures.
Insights from Pain Specialists and Sports Therapists
Leading pain management experts increasingly recognize CO₂ cryotherapy as a valuable addition to multimodal treatment approaches, particularly for patients seeking non-pharmacological alternatives. Sports medicine physicians report enhanced recovery rates and reduced injury recurrence in athletes utilizing CO₂ cryotherapy as part of comprehensive rehabilitation programs. Physical therapists note improved treatment tolerance and accelerated functional gains when cryotherapy precedes manual therapy or exercise interventions. Orthopedic surgeons have incorporated post-operative CO₂ cryotherapy protocols with reports of reduced opioid requirements and shortened recovery times. Rheumatologists observe sustained symptom improvement in arthritis patients receiving regular treatments, with some achieving medication dose reductions. Pain specialists emphasize the therapy’s value in breaking chronic pain cycles and reducing central sensitization patterns. The consensus among experts supports CO₂ cryotherapy’s integration into evidence-based treatment protocols while acknowledging the need for continued research to optimize parameters and patient selection criteria.
Real-World Case Studies
Clinical case studies provide valuable insights into CO₂ cryotherapy’s practical applications and therapeutic potential across diverse patient populations and conditions. A professional tennis player with chronic shoulder impingement experienced complete symptom resolution following an 8-week CO₂ cryotherapy protocol, enabling return to competitive play without medication. An elderly patient with severe knee osteoarthritis achieved 70% pain reduction and discontinued daily analgesics after 12 treatments over 6 weeks. A post-surgical patient following total knee replacement experienced accelerated rehabilitation and reduced swelling when CO₂ cryotherapy was initiated immediately post-operatively. A fibromyalgia patient with multiple tender points reported significant sleep improvement and reduced pain intensity following twice-weekly treatments over 3 months. A construction worker with chronic low back pain returned to full work capacity after combining CO₂ cryotherapy with physical therapy, avoiding planned surgical intervention. These cases illustrate the therapy’s versatility and potential for transformative outcomes across various clinical scenarios.
Integration with Other Modalities
Physical Therapy: Applying CO₂ cryotherapy before physical therapy sessions reduces pain and inflammation, improving tissue mobility and enhancing the effectiveness of manual therapy and exercise.
Ultrasound Therapy: Cryotherapy enhances tissue receptivity to ultrasound treatment, resulting in better anti-inflammatory and tissue-healing effects.
Acupuncture: Performing acupuncture after CO₂ cryotherapy can increase patient tolerance and promote more effective responses due to improved circulation and reduced muscle tension.
Massage Therapy: Pre-treatment cryotherapy allows for deeper, more comfortable massage work by relaxing tissues and decreasing pain sensitivity.
Pharmacological Pain Management: Regular cryotherapy sessions can reduce the required dosage of pain medications by enhancing their effects, helping minimize side effects while preserving therapeutic impact.
Final Thoughts on CO₂ Cryotherapy for Pain and Inflammation
La cryothérapie au CO₂ est a powerful, evidence-supported tool for managing pain and reducing inflammation. Research highlights its advantages over traditional cold therapies, including precise temperature control, rapid onset, improved comfort, and better clinical outcomes across varied patient populations. Its non-invasive nature and minimal side effects make it especially suitable for patients with drug sensitivities or those seeking non-pharmacological alternatives. The short treatment time and high tolerability improve patient adherence and streamline clinical workflows, particularly in fast-paced settings. As healthcare increasingly favors personalized, low-risk, and evidence-based approaches, CO₂ cryotherapy offers a safe, effective, and versatile option. Future research should focus on optimizing protocols, identifying ideal candidates, and exploring broader applications. Long-term studies and deeper mechanistic insights will help validate its sustained benefits. Effective integration depends on clinician training, careful patient selection, and setting realistic expectations to maximize therapeutic outcomes and ensure safe, successful use in comprehensive care programs.