Anterior cruciate ligament (ACL) reconstruction surgery represents one of the most challenging orthopedic procedures in terms of recovery time and patient outcomes. While traditional cold therapy has long been a cornerstone of post-surgical care, CO₂ cryotherapy is emerging as a cutting-edge alternative that promises superior pain management, reduced inflammation, and accelerated healing. This comprehensive guide explores how this innovative technology is transforming ACL recovery protocols.
Introduction: The ACL Surgery Recovery Challenge
The journey back to full functionality after ACL reconstruction is often longer and more complex than patients anticipate. Understanding the unique challenges of ACL recovery helps contextualize why advanced therapeutic interventions like CO₂ cryotherapy are becoming increasingly valuable in modern orthopedic care.
Why ACL Injuries Are Tough to Bounce Back From
ACL injuries affect approximately 400,000 Americans annually, with athletes representing a significant portion of these cases. The anterior cruciate ligament serves as a critical stabilizer within the knee joint, connecting the femur to the tibia and preventing excessive forward motion of the tibia relative to the femur. When this ligament is damaged, the resulting instability compromises not only athletic performance but also basic functional activities. The complexity of ACL recovery stems from multiple factors including the ligament’s poor blood supply, the intricate nature of knee biomechanics, and the substantial inflammatory response triggered by surgical reconstruction. Post-surgical complications such as arthrofibrosis, persistent pain, and delayed return to activity can significantly impact patient outcomes and quality of life.
Traditional Post-Surgery Protocols: Ice, Rest, Repeat
Conventional post-ACL surgery protocols have historically relied on the RICE methodology (Rest, Ice, Compression, Elevation) as the foundation of immediate post-operative care. Cryotherapy has been shown to have a statistically significant benefit in postoperative pain control, making it a standard component of recovery programs. Traditional ice therapy typically involves applying ice packs for 15-20 minutes every 2-3 hours during the initial post-operative period. While effective at reducing surface temperature and providing some pain relief, conventional ice application has limitations including inconsistent temperature delivery, skin protection requirements, and patient compliance challenges. The depth of tissue penetration with standard ice therapy is also relatively limited, potentially reducing its effectiveness on deeper inflammatory processes.

Where CO₂ Cryotherapy Fits in Today’s Recovery Landscape
Modern orthopedic rehabilitation increasingly emphasizes evidence-based interventions that can accelerate recovery while minimizing complications. CO₂ cryotherapy represents a significant advancement in therapeutic cold application, offering precise temperature control, deeper tissue penetration, and enhanced patient comfort compared to traditional methods. This technology utilizes pressurized carbon dioxide to deliver controlled, localized cooling that can reach temperatures of -78°C (-108°F) for brief periods. The precision and intensity of CO₂ cryotherapy allow for more targeted therapeutic effects, potentially reducing the overall treatment duration while maximizing clinical benefits. Integration of this technology into post-ACL surgery protocols represents a paradigm shift toward more sophisticated, patient-centered recovery approaches.
What Is CO₂ Cryotherapy?
Understanding the fundamental principles and mechanisms of CO₂ cryotherapy is essential for appreciating its therapeutic potential in post-ACL surgery care. This technology represents a significant evolution from traditional cold therapy applications, offering enhanced precision and therapeutic effectiveness.
The Science Behind CO₂ Cryotherapy
CO₂ cryotherapy, also known as neurocryostimulation, utilizes the rapid expansion of pressurized carbon dioxide to create intense, localized cooling. When pressurized CO₂ is released through a specialized nozzle, it undergoes rapid decompression and phase change, creating a focused stream of extremely cold gas that can reach temperatures of -78°C (-108°F). The physiological mechanism involves rapid vasoconstriction followed by reactive vasodilation, creating a “thermal shock” response that activates multiple healing pathways. The extreme cold triggers immediate analgesic effects through nerve conduction blockade, while the subsequent reperfusion phase enhances nutrient delivery and metabolic recovery. This dual-phase response provides both immediate symptomatic relief and longer-term healing benefits.
How It Differs from Traditional Cold Therapy
Unlike conventional ice therapy, which provides gradual, diffuse cooling, CO₂ cryotherapy delivers precise, instantaneous temperature reduction to targeted areas. The controlled nature of CO₂ application allows for consistent temperature delivery without the variability associated with melting ice or temperature fluctuations common with traditional methods. The penetration depth of CO₂ cryotherapy significantly exceeds that of standard ice application, reaching deeper tissue layers where post-surgical inflammation often persists. Additionally, the dry nature of CO₂ eliminates moisture-related skin complications, while the brief application time (typically 10-15 seconds) reduces the risk of tissue damage associated with prolonged cold exposure.
CO₂ Cryotherapy Devices Used in Orthopedic Rehab
Modern CO₂ cryotherapy systems feature sophisticated delivery mechanisms designed for clinical and home use applications. These devices typically include pressurized CO₂ cartridges, precision nozzles for targeted application, and safety features to prevent excessive exposure. Professional-grade units often incorporate digital controls, treatment timers, and ergonomic designs that facilitate patient positioning and treatment delivery. The portability and ease of use of contemporary CO₂ cryotherapy devices make them particularly suitable for integration into comprehensive ACL recovery protocols. Many systems are designed to be user-friendly, allowing patients to perform treatments independently under clinical supervision. The consistent performance and reliability of these devices contribute to improved treatment adherence and outcomes.
Safety Profile: Is It Too Cold to Be Safe?
Despite the extreme temperatures involved, CO₂ cryotherapy maintains an excellent safety profile when properly administered. The brief exposure time (typically 10-15 seconds) prevents tissue damage while maximizing therapeutic benefits. The rapid warming that follows CO₂ application minimizes the risk of frostbite or other cold-related injuries. Contraindications for CO₂ cryotherapy include open wounds, severe peripheral vascular disease, and cold hypersensitivity disorders. Patient selection and proper technique are crucial for maintaining safety while maximizing therapeutic effectiveness. Clinical supervision during initial treatments ensures proper application technique and patient tolerance assessment.
CO₂ Cryotherapy After ACL Surgery: Benefits That Matter
The therapeutic advantages of CO₂ cryotherapy in post-ACL surgery recovery extend beyond simple pain relief, encompassing multiple physiological processes that contribute to enhanced healing and functional restoration. Understanding these benefits helps optimize treatment protocols and patient expectations.
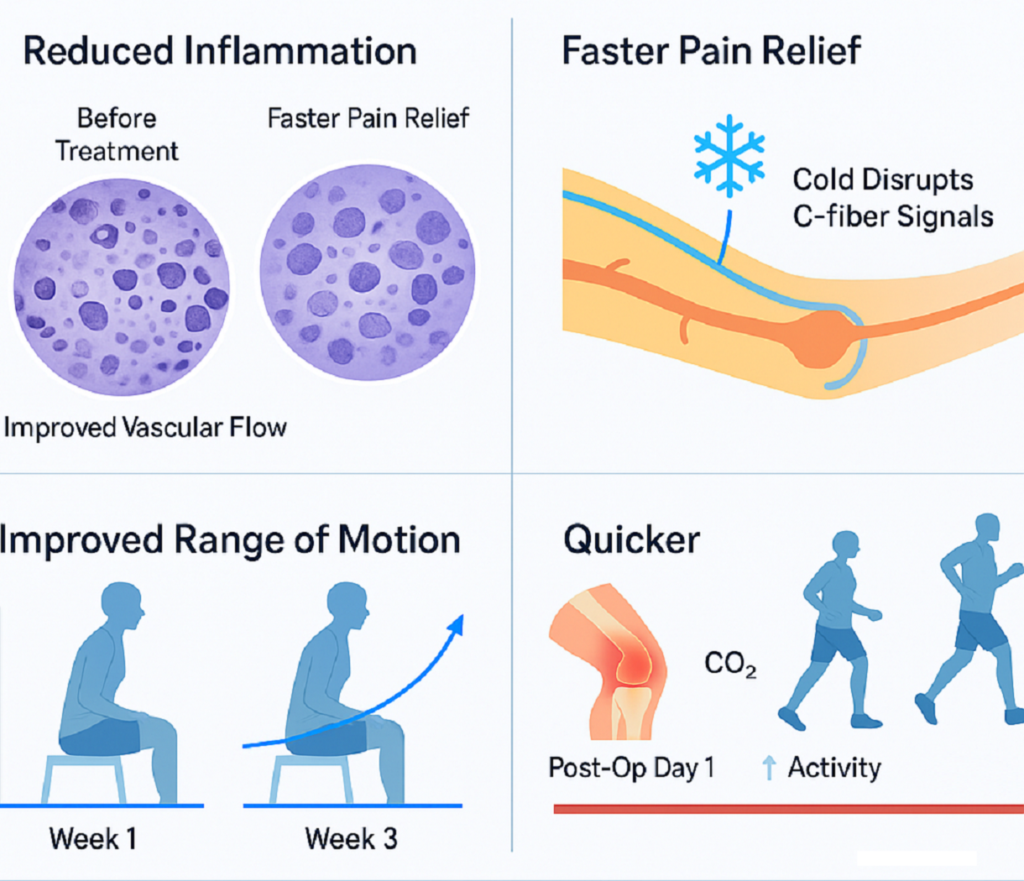
Reduced Post-Surgical Inflammation
Post-surgical inflammation represents one of the primary barriers to rapid ACL recovery. Cryotherapy promotes the reduction of pain, drug intake, length of hospital stay, the improvement of knee ROM and the patient’s quality of life. CO₂ cryotherapy’s intense cold application triggers immediate vasoconstriction, reducing inflammatory mediator accumulation in the surgical site. The anti-inflammatory effects of CO₂ cryotherapy extend beyond immediate vasoconstriction. The thermal shock response modulates inflammatory cytokine production, potentially reducing the overall inflammatory burden during the critical initial healing phase. This reduction in inflammatory activity can prevent secondary tissue damage and promote more efficient tissue repair processes.
Faster Pain Relief Without Drugs
Pain management represents a critical component of post-ACL surgery care, with implications for both patient comfort and rehabilitation progress. CO₂ cryotherapy provides immediate analgesic effects through multiple mechanisms, including nerve conduction blockade and endorphin release activation. Cryotherapy after arthroscopic anterior cruciate ligament reconstruction significantly reduced immediate post-surgery pain. The rapid onset of pain relief with CO₂ cryotherapy can reduce dependence on narcotic pain medications, potentially minimizing opioid-related side effects and complications. This non-pharmacological approach to pain management aligns with current trends toward multimodal analgesia and reduced opioid utilization in post-operative care.
Improved Range of Motion and Knee Flexibility
Joint stiffness and restricted range of motion represent common complications following ACL reconstruction, often requiring extensive physical therapy intervention. CO₂ cryotherapy’s anti-inflammatory effects can reduce joint capsule swelling and periarticular tissue restriction, facilitating earlier and more aggressive range of motion exercises. The muscle relaxation effects of CO₂ cryotherapy may also contribute to improved flexibility by reducing protective muscle spasm and allowing for more effective stretching and mobilization techniques. This enhanced flexibility can accelerate the return to functional activities and reduce the risk of long-term joint stiffness complications.
Shorter Downtime and Quicker Return to Activity
The combination of reduced inflammation, enhanced pain control, and improved range of motion contributes to accelerated overall recovery following ACL reconstruction. Patients undergoing CO₂ cryotherapy may experience shorter hospital stays, reduced rehabilitation duration, and earlier return to pre-injury activity levels. The enhanced healing environment created by CO₂ cryotherapy may also improve the quality of tissue repair, potentially reducing the risk of re-injury and long-term complications. This improved healing quality can translate to better long-term functional outcomes and reduced healthcare utilization.
When Cryotherapy Makes the Biggest Impact
The timing of CO₂ cryotherapy application significantly influences its therapeutic effectiveness. Maximum benefits are typically observed when treatments begin immediately post-operatively and continue throughout the acute inflammatory phase (first 48-72 hours). Early intervention can prevent the establishment of chronic inflammatory patterns and reduce the overall recovery timeline. Optimal treatment frequency typically involves multiple daily sessions during the first week post-surgery, with gradual reduction in frequency as healing progresses. Integration with other rehabilitation modalities, including physical therapy and progressive exercise programs, can maximize the synergistic effects of CO₂ cryotherapy.
How Does CO₂ Cryotherapy Actually Work on ACL Tissues?
The cellular and molecular mechanisms underlying CO₂ cryotherapy’s therapeutic effects provide insight into its superior clinical performance compared to traditional cold therapy approaches. Understanding these mechanisms helps optimize treatment protocols and patient selection.
Vasoconstriction and Controlled Reperfusion
The initial response to CO₂ cryotherapy involves rapid vasoconstriction of local blood vessels, reducing blood flow to the treated area and limiting inflammatory cell infiltration. This immediate vascular response helps contain the inflammatory process and prevents excessive tissue swelling that can impede healing. Following the initial vasoconstriction, reactive vasodilation occurs as tissues rewarm, creating a controlled reperfusion phase that enhances nutrient delivery and metabolic recovery. This biphasic vascular response optimizes the balance between inflammatory control and tissue healing, providing therapeutic benefits that extend beyond simple cold application.
Modulation of Nerve Signals for Pain Relief
CO₂ cryotherapy’s analgesic effects result from direct neural modulation through cold-induced nerve conduction blockade. The extreme cold temporarily disrupts pain signal transmission along nociceptive pathways, providing immediate relief from post-surgical discomfort. This neural blockade can persist for hours following brief CO₂ application. Additionally, the thermal shock response triggers endogenous opioid release and activates descending pain inhibitory pathways, creating a cascade of analgesic effects that complement the direct neural blockade. This multi-level pain modulation provides superior and longer-lasting pain relief compared to traditional cold therapy approaches.
Decreased Inflammatory Markers in Synovial Fluid
Research indicates that CO₂ cryotherapy can reduce inflammatory mediator concentrations in synovial fluid, including prostaglandins, leukotrienes, and inflammatory cytokines. This biochemical modulation contributes to reduced joint inflammation and improved healing environment within the knee joint. The reduction in inflammatory markers correlates with improved clinical outcomes, including reduced pain, enhanced range of motion, and accelerated functional recovery. Monitoring of inflammatory biomarkers can provide objective evidence of treatment effectiveness and guide therapeutic decision-making.
ATP Preservation and Muscle Regeneration
The metabolic effects of CO₂ cryotherapy extend to cellular energy preservation and enhanced muscle regeneration. Cold-induced metabolic depression can reduce cellular energy demand during the critical post-surgical period, preventing secondary tissue damage from metabolic stress. Enhanced muscle regeneration following CO₂ cryotherapy may result from improved satellite cell activation and reduced muscle fiber damage. This enhanced regenerative capacity can contribute to better functional outcomes and reduced long-term complications following ACL reconstruction.
Comparing the Cold: CO₂ Cryotherapy vs. Traditional Ice
Direct comparison between CO₂ cryotherapy and traditional ice therapy reveals significant differences in therapeutic effectiveness, patient comfort, and clinical outcomes. Understanding these differences helps guide treatment selection and optimize patient care.
Surface Temperature Drop Efficiency
CO₂ cryotherapy achieves significantly greater surface temperature reduction compared to traditional ice application. While ice therapy typically reduces skin temperature by 10-15°C, CO₂ cryotherapy can achieve temperature drops of 30-40°C within seconds of application. This enhanced cooling efficiency translates to more potent therapeutic effects. The rapid temperature reduction with CO₂ cryotherapy also allows for shorter treatment durations while maintaining therapeutic effectiveness. This efficiency advantage improves patient compliance and reduces treatment burden, particularly important during the intensive early recovery phase.
Duration and Depth of Tissue Penetration
The penetration depth of CO₂ cryotherapy significantly exceeds that of traditional ice therapy, reaching deeper tissue layers where post-surgical inflammation often persists. While ice therapy primarily affects superficial tissues, CO₂ cryotherapy can influence deeper structures including joint capsules, ligaments, and muscle tissue. The enhanced penetration depth of CO₂ cryotherapy allows for more comprehensive treatment of the inflammatory process, potentially reducing the overall treatment duration required to achieve clinical benefits. This deeper tissue effect may contribute to superior long-term outcomes compared to surface-only cooling approaches.
Skin Safety and Comfort Levels
Despite the extreme temperatures involved, CO₂ cryotherapy maintains superior skin safety compared to prolonged ice application. The brief exposure time prevents tissue damage while the dry nature of CO₂ eliminates moisture-related skin complications common with ice therapy. Patient comfort during CO₂ cryotherapy is generally superior to traditional ice application, with many patients reporting minimal discomfort during treatment. The absence of prolonged cold exposure and elimination of wet, uncomfortable ice packs contribute to improved patient tolerance and compliance.
Convenience and Consistency in Home Use
CO₂ cryotherapy devices offer superior convenience and consistency compared to traditional ice therapy for home use applications. The elimination of ice preparation, storage, and replacement requirements simplifies treatment protocols and improves patient adherence to prescribed therapy regimens. The consistent performance of CO₂ cryotherapy devices ensures reliable therapeutic delivery regardless of user technique or environmental conditions. This consistency advantage is particularly important for maintaining treatment effectiveness throughout the extended recovery period following ACL reconstruction.
Who Should Consider CO₂ Cryotherapy After ACL Surgery?
Patient selection for CO₂ cryotherapy involves careful consideration of individual factors including activity level, recovery goals, and medical history. Understanding optimal candidate characteristics helps maximize treatment effectiveness and minimize complications.
Athletes and Active Individuals
Athletes and highly active individuals represent ideal candidates for CO₂ cryotherapy due to their demanding recovery timelines and performance expectations. The enhanced healing environment created by CO₂ cryotherapy can facilitate faster return to sport and reduced risk of re-injury. The superior pain control and anti-inflammatory effects of CO₂ cryotherapy align with the intensive rehabilitation requirements of athletic populations. Early return to training and competition activities often depends on rapid resolution of post-surgical inflammation and restoration of functional capacity.
Patients with Opioid Sensitivities
Individuals with opioid sensitivities or addiction concerns benefit significantly from CO₂ cryotherapy’s non-pharmacological pain management approach. The substantial analgesic effects of CO₂ cryotherapy can reduce or eliminate the need for narcotic pain medications during the critical initial recovery period. The multimodal pain management approach facilitated by CO₂ cryotherapy aligns with current best practices for opioid-sparing anesthesia and post-operative care. This approach can reduce healthcare costs and improve patient satisfaction while maintaining effective pain control.
Older Adults Needing Faster Functional Recovery
Older adults undergoing ACL reconstruction often face unique challenges including delayed healing, increased complication risk, and functional decline during prolonged recovery periods. CO₂ cryotherapy’s enhanced healing environment can be particularly beneficial for this population. The reduced inflammatory burden and enhanced pain control provided by CO₂ cryotherapy can facilitate earlier mobilization and more aggressive rehabilitation in older adults. This accelerated recovery approach can prevent complications associated with prolonged immobilization and improve long-term functional outcomes.
Not for Everyone: Contraindications and Cautions
Certain patient populations may not be suitable candidates for CO₂ cryotherapy due to increased risk of complications or reduced therapeutic effectiveness. Contraindications include severe peripheral vascular disease, open wounds at the treatment site, and cold hypersensitivity disorders. Patients with compromised immune systems, diabetes with poor circulation, or history of adverse reactions to cold therapy require careful evaluation before initiating CO₂ cryotherapy. Clinical assessment and medical clearance ensure safe and effective treatment delivery.

Real-World Evidence: What the Research and Experts Say
The clinical evidence supporting CO₂ cryotherapy in post-ACL surgery care continues to evolve, with emerging research demonstrating promising therapeutic advantages. Understanding the current evidence base helps inform clinical decision-making and treatment protocols.
Clinical Trials on CO₂ Cryotherapy for ACL Recovery
Recent studies have investigated the effect of cryotherapy with carbon dioxide hydrate on fatigue recovery of neuromuscular function and muscle blood circulation. While specific large-scale randomized controlled trials focusing exclusively on CO₂ cryotherapy for ACL recovery remain limited, existing evidence suggests significant therapeutic potential. Preliminary studies indicate that CO₂ cryotherapy may offer superior pain control and faster functional recovery compared to traditional cold therapy approaches. The enhanced tissue penetration and controlled thermal effects of CO₂ cryotherapy appear to provide more comprehensive therapeutic benefits than conventional ice application.
Testimonials from Sports Physiatrists and Orthopedic Surgeons
Clinical experience from orthopedic surgeons and sports medicine specialists increasingly supports the integration of CO₂ cryotherapy into post-ACL surgery protocols. Practitioners report improved patient satisfaction, reduced pain medication requirements, and accelerated return to activity timelines with CO₂ cryotherapy implementation. The precision and consistency of CO₂ cryotherapy delivery have garnered particular praise from clinicians who appreciate the standardized treatment approach and reproducible therapeutic effects. Many practitioners report that CO₂ cryotherapy has become an essential component of their post-operative care protocols.
Research Gaps: What We Still Need to Know
Despite promising preliminary evidence, significant research gaps remain regarding optimal CO₂ cryotherapy protocols, long-term outcomes, and comparative effectiveness studies. Future research should focus on standardized treatment protocols, dosing parameters, and integration with other rehabilitation modalities. Large-scale randomized controlled trials comparing CO₂ cryotherapy to traditional cold therapy approaches are needed to establish definitive evidence for clinical superiority. Additionally, cost-effectiveness analyses and long-term outcome studies will help inform healthcare policy and insurance coverage decisions.
Patient Guide: What to Expect from CO₂ Cryotherapy
Understanding the patient experience with CO₂ cryotherapy helps set appropriate expectations and optimize treatment outcomes. Proper preparation and education contribute to successful treatment implementation and patient satisfaction.
How Sessions Work: Duration, Frequency, Feel
Typical CO₂ cryotherapy sessions involve brief applications (10-15 seconds) of focused cold therapy to the surgical site. Treatment frequency usually begins with multiple daily sessions during the first 48-72 hours post-surgery, with gradual reduction in frequency as healing progresses. Patients typically describe the sensation as an intense but tolerable cold feeling, followed by rapid warming and often immediate pain relief. The brief treatment duration minimizes discomfort while maximizing therapeutic benefits. Most patients find CO₂ cryotherapy more comfortable than prolonged ice pack application.
Side Effects: What’s Normal, What’s Not
Normal responses to CO₂ cryotherapy include temporary skin redness, mild tingling sensations, and immediate pain relief. These effects typically resolve within minutes of treatment completion and indicate appropriate therapeutic response. Abnormal responses requiring immediate medical attention include severe skin irritation, persistent numbness, or signs of tissue damage. Proper technique and appropriate patient selection minimize the risk of adverse effects while maximizing therapeutic benefits.
Tips for Maximizing Results
Optimal outcomes with CO₂ cryotherapy require adherence to prescribed treatment protocols and integration with comprehensive rehabilitation programs. Patients should maintain consistent treatment schedules, especially during the critical initial recovery period. Combining CO₂ cryotherapy with appropriate rest, elevation, and physical therapy exercises can enhance overall treatment effectiveness. Patient education regarding proper positioning, treatment timing, and activity modification contributes to successful outcomes.
Final Verdict: Should You Freeze Your Knee Back to Health?
The decision to incorporate CO₂ cryotherapy into post-ACL surgery care requires careful consideration of individual patient factors, treatment goals, and available resources. Understanding the benefits and limitations helps guide informed treatment decisions.
Pros and Cons of CO₂ Cryotherapy Post-ACL Surgery
Advantages of CO₂ cryotherapy include superior pain control, enhanced anti-inflammatory effects, improved patient comfort, and potential for accelerated recovery. The precision and consistency of treatment delivery provide therapeutic advantages over traditional cold therapy approaches. Potential disadvantages include higher initial costs, need for specialized equipment, and limited long-term outcome data. Patient selection and proper technique are crucial for optimizing benefits while minimizing risks and costs.
Who Gets the Most Benefit?
Patients most likely to benefit from CO₂ cryotherapy include athletes, individuals with demanding recovery timelines, and those seeking to minimize pain medication use. The enhanced therapeutic effects of CO₂ cryotherapy align particularly well with intensive rehabilitation requirements and performance expectations. Optimal candidates typically have realistic expectations, good overall health, and commitment to comprehensive rehabilitation programs. The integration of CO₂ cryotherapy into evidence-based recovery protocols can maximize therapeutic benefits and improve long-term outcomes.
FAQs About CO₂ Cryotherapy and ACL Recovery
CO₂ cryotherapy delivers ultra-rapid cooling through carbon dioxide jets that penetrate deeper and more uniformly than ice packs. Unlike melting ice, it maintains a controlled temperature without causing tissue freezing, giving you therapeutic effects without the soggy towel aftermath.
Many patients report reduced reliance on opioids or NSAIDs when using CO₂ cryotherapy regularly post-surgery. It works by modulating nerve pain signals and decreasing inflammation. While not always a complete replacement, it often reduces dosage and duration significantly.
Not hype—just smart biology. By reducing joint swelling and muscle inhibition, CO₂ cryotherapy helps restore range of motion and neuromuscular control faster. That means you may start rehab exercises sooner and with less discomfort, accelerating your return to action.
Yes, many CO₂ cryotherapy systems are designed for safe at-home use with built-in temperature controls and timers. However, it’s best to follow a physiotherapist-recommended protocol, especially in the early post-op weeks when the tissue is most vulnerable.
Yes—and sometimes even better. Older adults tend to experience prolonged inflammation and slower circulation, which cryotherapy directly targets. The gentle, drug-free relief it provides is especially helpful for seniors who may not tolerate NSAIDs well.
Great question. CO₂ cryotherapy is gaining popularity, but barriers like cost, clinician familiarity, and access to devices have slowed adoption. As more studies support its benefits, it’s becoming a go-to tool in elite sports rehab and progressive clinics.



