Why Soft Tissue Inflammation Stops You in Your Tracks
Soft tissue inflammation is a widespread condition that affects millions, disrupting mobility, productivity, and overall well-being. Though inflammation is a natural healing response, it can become chronic—leading to persistent pain, tissue damage, and disability. Common causes include sports injuries, repetitive strain, surgery, and chronic conditions. When the inflammatory process becomes dysregulated, it often resists traditional treatment. Standard anti-inflammatory therapies like NSAIDs or corticosteroids can offer temporary relief but are often limited by side effects, dependency risks, and poor long-term results. As a result, there’s growing demand for alternative therapies that are both safe and effective. CO₂ cryotherapy has emerged as a promising option—offering targeted, non-invasive relief by reducing inflammation and supporting tissue recovery, without the downsides of systemic medications. With healthcare systems burdened by inflammation-related conditions, innovative approaches like this are increasingly needed.
What Exactly Is CO₂ Cryotherapy and How Does It Work?
Understanding the mechanisms and applications of CO₂ cryotherapy requires a comprehensive examination of its physiological effects and therapeutic principles. This innovative treatment modality represents a significant advancement in targeted therapeutic interventions for inflammatory conditions.
O que é a crioterapia com CO₂?
CO₂ cryotherapy utilizes pressurized carbon dioxide delivered through specialized devices to create precise, controlled therapeutic cooling at temperatures reaching -78°C (-108°F). The treatment involves direct application of CO₂ gas to affected tissues for brief periods, typically 10-15 seconds per application site, creating rapid vasoconstriction followed by reactive hyperemia. This precise temperature control allows for targeted treatment of specific anatomical regions without affecting surrounding healthy tissue. The carbon dioxide is stored in pressurized cartridges and delivered through specialized applicators that ensure consistent temperature delivery and safety protocols. Unlike traditional ice applications or whole-body cryotherapy, CO₂ cryotherapy provides localized treatment with immediate onset of therapeutic effects and minimal patient discomfort.
The Physiological Impact of CO₂ Cryotherapy
The physiological mechanisms underlying CO₂ cryotherapy’s therapeutic effects involve multiple interconnected pathways that collectively contribute to reduced inflammation and enhanced healing. The extreme cold temperature triggers immediate vasoconstriction, reducing blood flow to the treated area and limiting the delivery of inflammatory mediators. This is followed by reactive vasodilation, which enhances circulation and promotes the removal of metabolic waste products and inflammatory debris. The cold stimulus activates the gate control theory of pain modulation, where large-diameter nerve fibers block pain signals transmitted by smaller nociceptive fibers. Additionally, the thermal shock stimulates the release of endorphins and other endogenous analgesic compounds, providing natural pain relief that can persist beyond the immediate treatment period.

Common Causes and Signs of Soft Tissue Inflammation
To fully appreciate the therapeutic potential of CO₂ cryotherapy, it’s essential to understand the diverse spectrum of conditions that involve soft tissue inflammation and the challenges associated with their conventional management. This understanding provides the foundation for evaluating innovative treatment approaches.
Causes and Common Conditions
- Acute traumatic injuries, including contusions, strains, and sprains, represent the most common cause of inflammatory responses in muscles, tendons, and ligaments.
- Overuse syndromes, particularly prevalent in athletic populations and occupational settings, result from repetitive microtrauma that overwhelms the tissue’s repair capacity.
- Degenerative conditions such as tendinopathies and arthritis involve chronic inflammatory processes that can persist for months or years.
- Autoimmune conditions including rheumatoid arthritis and systemic lupus erythematosus create systemic inflammatory responses that affect multiple tissue types.
- Post-surgical inflammation, while often necessary for healing, can become problematic when excessive or prolonged.
Symptoms and Diagnosis Challenges
The clinical presentation of soft tissue inflammation encompasses a constellation of symptoms that can vary significantly in intensity, duration, and functional impact. The classic signs include dolor (pain), rubor (redness), calor (heat), tumor (swelling), and functio laesa (loss of function), collectively representing the cardinal signs of inflammation first described by Celsus and Virchow. Pain typically presents as a deep, aching sensation that may be constant or activity-related, often accompanied by tenderness to palpation and increased sensitivity to movement. Edema formation results from increased vascular permeability and can lead to tissue distortion and mechanical dysfunction. Diagnostic challenges arise from the subjective nature of pain assessment, variable inflammatory markers, and the need to differentiate between acute and chronic inflammatory states. Advanced imaging techniques including ultrasound, MRI, and infrared thermography may be required for accurate assessment and monitoring of treatment responses.
The Limitations of Traditional Treatments
Conventional anti-inflammatory treatments, while forming the cornerstone of current therapeutic approaches, present significant limitations that have prompted the search for alternative modalities. Nonsteroidal anti-inflammatory drugs (NSAIDs) provide effective symptom relief but carry risks of gastrointestinal ulceration, cardiovascular complications, and renal dysfunction, particularly with prolonged use. Corticosteroid injections offer potent anti-inflammatory effects but may cause tissue atrophy, delayed healing, and systemic side effects. Physical therapy interventions, while beneficial for functional restoration, may be limited by patient tolerance during acute inflammatory phases. Traditional ice applications provide temporary relief but lack the precision and depth of penetration necessary for optimal therapeutic outcomes. The challenge lies in finding treatments that can provide rapid, effective anti-inflammatory effects while minimizing adverse reactions and promoting natural healing processes.
How CO₂ Cryotherapy Stands Out: Benefits and Science Behind It
The unique mechanisms and therapeutic advantages of CO₂ cryotherapy distinguish it from conventional anti-inflammatory treatments, offering a promising alternative for patients seeking effective, non-pharmacological interventions for soft tissue inflammation.
Mechanisms Behind Anti-Inflammatory Action
CO₂ cryotherapy’s anti-inflammatory effects operate through multiple interconnected pathways that target key components of the inflammatory cascade. The extreme cold temperature causes immediate vasoconstriction, reducing the delivery of inflammatory mediators including prostaglandins, leukotrienes, and cytokines to the affected tissues. This vasoconstriction also limits the extravasation of inflammatory cells, particularly neutrophils and macrophages, which are primary contributors to tissue damage and prolonged inflammation. The thermal shock activates cold-sensitive ion channels, particularly TRPM8 receptors, which modulate inflammatory signaling pathways and reduce the production of pro-inflammatory mediators. Additionally, the cold stimulus triggers the release of norepinephrine and other catecholamines, which have direct anti-inflammatory effects through α-adrenergic receptor activation. The subsequent reactive hyperemia phase enhances lymphatic drainage, facilitating the removal of inflammatory debris and metabolic waste products that perpetuate the inflammatory response.
Pain Reduction and Enhanced Healing
The analgesic effects of CO₂ cryotherapy result from multiple mechanisms that provide both immediate and sustained pain relief. The cold temperature reduces nerve conduction velocity, particularly in pain-transmitting C-fibers and A-delta fibers, effectively blocking nociceptive signals from reaching the central nervous system. This neural blockade provides immediate pain relief that can persist for hours following treatment. The activation of the gate control mechanism, where large-diameter mechanoreceptors inhibit pain transmission at the spinal cord level, contributes to prolonged analgesia. Enhanced healing occurs through improved circulation following the initial vasoconstriction phase, which increases oxygen and nutrient delivery to damaged tissues. The cold stimulus also promotes the release of growth factors and cytokines that facilitate tissue repair and regeneration. Additionally, the reduction in inflammatory cell infiltration prevents secondary tissue damage and creates an optimal environment for healing.
Clinical Advantages Over Conventional Therapies
- Precise, Localized Targeting: CO₂ cryotherapy directly treats inflamed tissues without affecting the rest of the body.
- No Systemic Side Effects: It avoids drug-related issues such as gastrointestinal upset, cardiovascular risks, or medication interactions.
- Rapid Onset of Relief: Patients often feel therapeutic effects immediately after treatment.
- Short Treatment Time: Each application lasts only 10–15 seconds, making it efficient for both patients and clinicians.
- Repeatable Without Harm: Can be safely used multiple times without cumulative damage or toxicity.
- Tissue-Friendly Compared to Steroids: Unlike corticosteroid injections, it doesn’t hinder healing or damage joint and soft tissue structures.
- Non-Invasive and Low Risk: No needles, no incisions—minimizing infection risk and requiring zero downtime.
- Consistent, Controlled Delivery: Built-in temperature control and standardized protocols ensure reliable results across providers.
Evidence-Based Insights: What Does Research Say?
The scientific foundation supporting CO₂ cryotherapy for soft tissue inflammation continues to evolve, with emerging research providing valuable insights into its therapeutic mechanisms, clinical efficacy, and optimal application protocols. This evidence base is crucial for establishing the role of CO₂ cryotherapy in contemporary anti-inflammatory treatment paradigms.
Review of Key Clinical Trials and Studies
Emerging research supports the efficacy of CO₂ cryotherapy in managing inflammation, though the field is still developing. A notable randomized controlled trial found that patients with acute ankle sprains experienced greater reductions in pain, swelling, and disability when treated with CO₂ cryotherapy compared to traditional ice therapy. Participants also returned to normal activity faster and required fewer pain medications. Laboratory studies show that CO₂ cryotherapy lowers inflammatory biomarkers like CRP, IL-6, and TNF-α. Thermal imaging confirms reduced heat and improved circulation post-treatment. Additionally, comparative studies reveal deeper tissue penetration and longer-lasting effects than conventional cold therapy. While these findings are promising, more robust evidence—particularly large-scale, multi-center trials—is needed to confirm long-term safety and efficacy.
Real-World Outcomes and Patient Testimonials
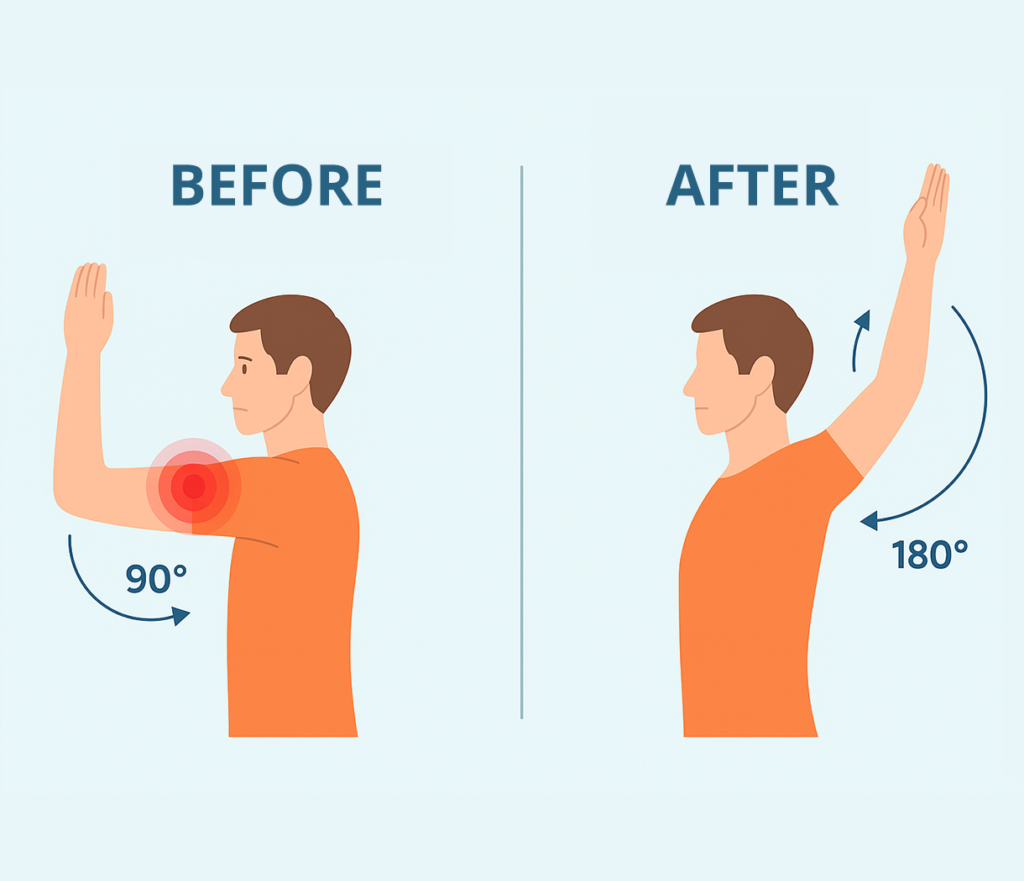
In clinical practice, CO₂ cryotherapy has demonstrated strong real-world benefits. Sports medicine experts report shorter recovery times and quicker returns to competition after acute injuries. Patients with chronic inflammation, such as tendinopathy or arthritis, frequently experience long-term pain relief and improved mobility. Physical therapists who incorporate CO₂ cryotherapy into rehab protocols observe enhanced outcomes and higher patient satisfaction. Surveys show patients favor CO₂ cryotherapy for its comfort, rapid relief, and lack of systemic side effects—especially those who cannot tolerate NSAIDs or corticosteroids. Clinicians appreciate the simplicity of application and fast onset of results. Overall, CO₂ cryotherapy is emerging as a patient-friendly, well-tolerated solution with clear therapeutic value across various inflammatory conditions.
Gaps and Future Directions in Research
Despite encouraging early results, CO₂ cryotherapy research still faces key knowledge gaps. Optimal treatment parameters—such as duration, frequency, and temperature—are yet to be standardized. Long-term safety data is limited, particularly regarding repeated use over months or years. Comparative studies with standard anti-inflammatory treatments are essential for validating its clinical positioning. Basic science research on its cellular and molecular effects could uncover biomarkers for better patient targeting. In addition, cost-effectiveness analyses could determine its value relative to existing therapies. Research on combined approaches—such as pairing CO₂ cryotherapy with physical therapy or laser treatment—could enhance efficacy. Expanding the evidence base through well-designed trials will be vital to firmly establish CO₂ cryotherapy as a mainstream anti-inflammatory intervention.
Integrative Approach: Combining CO₂ Cryotherapy with Holistic Care
The optimal management of soft tissue inflammation requires a comprehensive, multi-modal approach that addresses not only the inflammatory process but also the underlying factors contributing to tissue dysfunction and the patient’s overall health and well-being. CO₂ cryotherapy represents one component of this integrative strategy.
Synergistic Use with Physical Therapy and Exercise
Combining CO₂ cryotherapy with physical therapy offers a powerful, synergistic approach to treating soft tissue inflammation. The therapy’s rapid pain relief and anti-inflammatory effects reduce muscle guarding, making manual therapy and stretching more effective. Applying CO₂ cryotherapy before treatment sessions can improve patient comfort and tolerance for challenging exercises. It also enhances circulation, boosting tissue oxygenation and nutrient delivery—creating an ideal environment for healing and physical adaptation. After exercise, CO₂ cryotherapy can help manage post-activity inflammation and speed up recovery. This integrated approach supports progressive tissue loading while minimizing flare-ups, potentially shortening recovery time and improving functional outcomes. Many physical therapists report higher patient engagement and better compliance with rehab programs when CO₂ cryotherapy is used as an adjunct treatment.
Lifestyle and Nutritional Support
- Adopt an Anti-Inflammatory Diet: Increase intake of omega-3s, antioxidants, fruits, and vegetables while reducing processed and sugary foods to lower systemic inflammation.
- Stay Well Hydrated: Proper hydration supports lymphatic drainage and helps flush out inflammatory byproducts and toxins.
- Prioritize Quality Sleep: Deep, restorative sleep is essential for immune function and soft tissue repair—lack of sleep worsens inflammation.
- Manage Stress Effectively: Practices like meditation, deep breathing, and yoga can calm the nervous system and reduce stress-induced inflammatory responses.
- Exercise Regularly (and Wisely): Low-impact, consistent movement enhances circulation and prevents stiffness while supporting long-term tissue health.
- Educate on Ergonomics and Activity Modifications: Proper posture, joint protection, and injury prevention strategies reduce mechanical strain and lower reinjury risk.
Patient Education: Setting Realistic Expectations
Clear patient education is essential for successful outcomes with CO₂ cryotherapy. Patients should know that this treatment works best when combined with other therapies, not as a standalone fix. While many feel immediate relief, lasting anti-inflammatory benefits often require multiple sessions over several weeks. It’s important to set realistic expectations about the timeline, frequency, and degree of improvement. Though side effects are rare, patients should be informed of possible temporary redness, numbness, or sensitivity at the treatment site. Educating patients on activity modifications and post-treatment care helps support healing. Emphasizing the therapy’s role within a broader recovery plan encourages better understanding and long-term compliance. When patients know what to expect—and what’s expected of them—they’re more likely to stay engaged, follow through, and achieve optimal results.
Conclusion: Is CO₂ Cryotherapy Ready to Lead the Way?
CO₂ cryotherapy is emerging as a promising tool for managing soft tissue inflammation, offering rapid relief, precise targeting, and minimal side effects. Its mechanisms—vasoconstriction, reduced inflammatory mediator activity, improved lymphatic drainage, and pain modulation—are well supported by early research. Clinicians and patients alike report positive outcomes, especially when used as part of a broader, multi-modal treatment plan. While larger, long-term studies are still needed to confirm its full potential and refine usage protocols, current evidence points to its value as a safe, effective, and non-invasive option. As healthcare trends shift toward personalized, non-pharmacological interventions, CO₂ cryotherapy is well-positioned to become a key player in future inflammation care strategies. Though not yet the universal first-line solution, it’s clearly a powerful contender in the evolving landscape of soft tissue therapy.
FAQs: Your Top Questions Answered
CO₂ cryotherapy uses controlled carbon dioxide to deliver faster, deeper, and more precise cooling—without the mess or uneven results of ice packs.
Most patients describe a brief cooling sensation that fades quickly. There’s no need for needles, incisions, or anesthesia.
Many experience relief within minutes of the first session, though optimal anti-inflammatory effects usually build up over several treatments.
Not necessarily—it works best when combined with physical therapy, exercise, and healthy lifestyle changes as part of a multi-modal approach.
Yes, studies and real-world use show positive outcomes for both acute injuries and chronic inflammation-related conditions.
If you’re struggling with soft tissue pain and want a drug-free, non-invasive option, this therapy might be a great fit. A clinician can help assess suitability.



