En el vertiginoso mundo de la medicina deportiva y la rehabilitación, la búsqueda de una recuperación más rápida de las lesiones impulsa la innovación continua en los enfoques terapéuticos. Las distensiones y los esguinces son algunas de las lesiones musculoesqueléticas más frecuentes, y afectan tanto a los deportistas de élite como a los guerreros de fin de semana. Los métodos de tratamiento tradicionales, aunque eficaces, a menudo requieren semanas o incluso meses para una recuperación completa, lo que deja a los pacientes frustrados y deseosos de alternativas. Llega la crioterapia con CO₂, un tratamiento de vanguardia que promete revolucionar la recuperación de las lesiones mediante la aplicación precisa de dióxido de carbono extremadamente frío. Esta avanzada modalidad terapéutica afirma que acelera la curación, reduce el dolor y restablece las funciones más rápidamente que los métodos convencionales, pero ¿apoya la ciencia estas audaces afirmaciones?
Introducción
Para comprender el potencial de la crioterapia de CO₂ es necesario examinar tanto la naturaleza de las lesiones comunes de los tejidos blandos como el panorama en evolución de las intervenciones terapéuticas diseñadas para optimizar los resultados de la recuperación. Este exhaustivo análisis explorará si este innovador tratamiento cumple realmente sus promesas.
¿Qué son las distensiones y los esguinces?
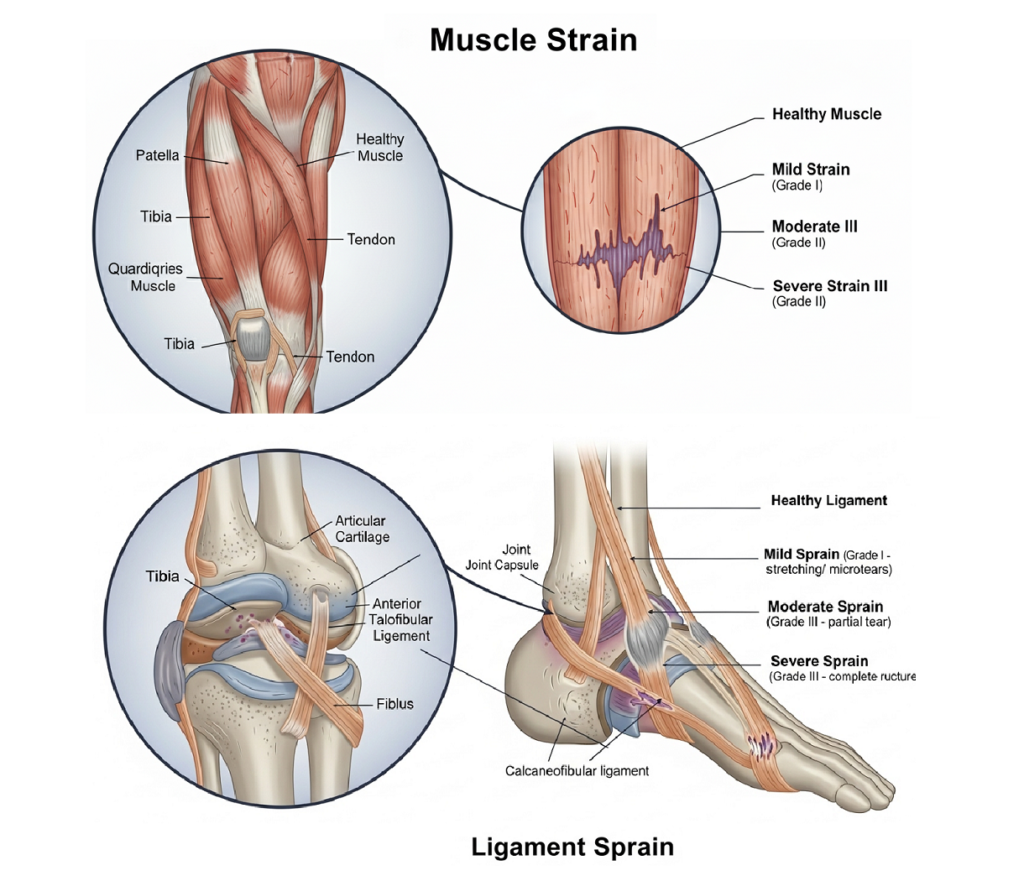
Las distensiones y los esguinces representan categorías distintas de lesiones de los tejidos blandos que afectan a estructuras anatómicas diferentes pero comparten mecanismos fisiopatológicos similares. Una distensión se produce cuando las fibras musculares o los tendones se estiran en exceso o se desgarran, lo que suele deberse a contracciones bruscas, cargas excéntricas o fatiga muscular. Estas lesiones afectan a la unidad músculo-tendinosa y pueden ir desde la rotura microscópica de fibras (Grado I) hasta la rotura completa (Grado III). Los esguinces son lesiones de los ligamentos -los tejidos conjuntivos fibrosos que conectan el hueso con el hueso- causadas por un movimiento de la articulación que supera la amplitud normal de movimiento. Al igual que las distensiones, los esguinces se clasifican según su gravedad: el Grado I implica un estiramiento leve, el Grado II un desgarro parcial y el Grado III una rotura completa del ligamento. Ambos tipos de lesión desencadenan cascadas inflamatorias, daño tisular y deterioro funcional que requieren una intervención terapéutica específica.
Por qué la velocidad de recuperación es importante para los deportistas y las personas activas
La velocidad de recuperación de las distensiones y los esguinces tiene profundas implicaciones para el rendimiento deportivo, la longevidad profesional y la calidad de vida de las personas activas. Los deportistas profesionales se ven sometidos a una enorme presión para volver rápidamente a la competición, ya que una ausencia prolongada puede afectar a la dinámica del equipo, las negociaciones contractuales y la trayectoria profesional. Los atletas aficionados y los entusiastas del fitness también dan prioridad a una recuperación rápida para mantener la constancia en el entrenamiento, evitar el desacondicionamiento y conservar la motivación para seguir participando. Los periodos de recuperación prolongados aumentan el riesgo de complicaciones secundarias, como atrofia muscular, rigidez articular, desacondicionamiento cardiovascular e impactos psicológicos como depresión y ansiedad. Además, el retraso en la curación puede dar lugar a patrones de movimiento compensatorios que predisponen a las personas a sufrir más lesiones. Las implicaciones económicas son considerables, ya que la pérdida de productividad laboral, los costes sanitarios y la posible discapacidad a largo plazo suponen una importante carga financiera para las personas y la sociedad.
El auge de la crioterapia con CO₂ en medicina deportiva
CO₂ crioterapia ha surgido como una modalidad terapéutica revolucionaria en medicina deportiva, ganando popularidad entre equipos profesionales, centros de rehabilitación y clínicas de optimización del rendimiento de todo el mundo. Esta forma avanzada de crioterapia utiliza dióxido de carbono a presión suministrado a temperaturas extremadamente bajas para crear efectos terapéuticos específicos que superan los métodos tradicionales de aplicación de hielo. La tecnología ha evolucionado de los laboratorios a la práctica clínica, con una creciente adopción impulsada por los prometedores resultados preliminares y los testimonios de los atletas. A diferencia de las cámaras de crioterapia para todo el cuerpo, la crioterapia con CO₂ permite un tratamiento localizado preciso, lo que la hace ideal para tratar lesiones específicas. La creciente reputación del tratamiento se debe a su capacidad para proporcionar un alivio inmediato del dolor, reducir la inflamación y acelerar potencialmente el proceso de curación a través de sofisticados mecanismos fisiológicos. A medida que siguen surgiendo nuevas investigaciones, los profesionales de la medicina deportiva incorporan cada vez más la crioterapia con CO₂ a los protocolos de tratamiento integral de las afecciones musculoesqueléticas agudas y crónicas.
Comprender las distensiones y los esguinces
Para apreciar plenamente cómo la crioterapia con CO₂ puede mejorar la curación, primero debemos comprender la compleja fisiopatología de las distensiones y los esguinces, incluidos sus mecanismos subyacentes, presentaciones clínicas y procesos naturales de curación. Esta base es crucial para evaluar las intervenciones terapéuticas.
Diferencia entre distensiones musculares y esguinces de ligamentos
| Característica | Distensiones musculares | Esguinces de ligamentos |
| Estructura anatómica afectada | Fibras musculares (actina, miosina) y matrices de tejido conjuntivo (endomisio, perimisio, epimisio) | Ligamentos compuestos de colágeno de tipo I |
| Sitio vulnerable | Unión músculo-tendinosa | Ligamento midsubstance con vascularidad limitada |
| Mecanismo de lesión | Típicamente durante contracciones excéntricas con alargamiento muscular forzado | Carga de tracción excesiva o movimiento anormal de la articulación |
| Propiedades biomecánicas | Tejido contráctil con gran adaptabilidad a la carga | Tejido no contráctil con resistencia a la tracción y viscoelasticidad |
| Capacidad de curación | Un suministro vascular relativamente mejor favorece la recuperación | La vascularidad limitada ralentiza la reparación y prolonga la recuperación |
Causas comunes: Lesiones deportivas, uso excesivo, mala condición física
- Los cambios bruscos de dirección, los saltos, los aterrizajes o los impactos directos pueden superar la tolerancia de los tejidos y provocar lesiones agudas.
- Las lesiones por uso excesivo son el resultado de microtraumatismos repetitivos que superan la capacidad de reparación de los tejidos.
- Un mal acondicionamiento, que incluya desequilibrios musculares, poca flexibilidad y un control neuromuscular débil, aumenta el riesgo de lesiones.
- Los factores ambientales, como las condiciones de la superficie, el diseño del equipo y las condiciones meteorológicas, pueden influir en la probabilidad de sufrir lesiones.
- Las anomalías biomecánicas como las discrepancias en la longitud de las piernas, la pronación del pie o una mecánica de movimiento alterada crean cargas de estrés anormales.
- Las lesiones previas, una rehabilitación inadecuada y el retorno prematuro a la actividad aumentan significativamente el riesgo de volver a lesionarse.
Síntomas que indican distensiones o esguinces
- En el momento de la lesión suele aparecer un dolor agudo y localizado o una sensación de desgarro.
- Se produce una rápida hinchazón debido a la permeabilidad vascular y a la liberación de mediadores inflamatorios.
- Los hematomas pueden aparecer en cuestión de horas o días, mostrando cambios de color que van del rojo al morado y al amarillo verdoso.
- Las distensiones musculares suelen cursar con sensibilidad, espasmos y debilidad durante los movimientos en tensión.
- Los esguinces suelen causar inestabilidad articular, reducción de la amplitud de movimiento y dolor al soportar peso.
- Las pruebas funcionales pueden revelar pérdida de fuerza, déficits propioceptivos y patrones de movimiento compensatorios.
- Las lesiones graves pueden cursar con deformidad, pérdida total de función o incapacidad para soportar peso.
Calendario típico de curación sin intervención
El proceso natural de curación de las distensiones y los esguinces sigue fases predecibles con acontecimientos celulares y moleculares específicos que determinan los plazos de recuperación y los resultados funcionales. La fase inflamatoria (0-72 horas) comienza inmediatamente con la hemostasia, la agregación plaquetaria y el reclutamiento de células inflamatorias como neutrófilos, macrófagos y linfocitos. Citoquinas proinflamatorias como el factor de necrosis tumoral alfa (TNF-α), la interleucina-1β (IL-1β) y la interleucina-6 (IL-6) orquestan la respuesta inicial al tiempo que ponen en marcha mecanismos de reparación tisular. La fase proliferativa (3-21 días) implica la migración de fibroblastos, la síntesis de colágeno, la angiogénesis y la formación de tejido de granulación. Inicialmente predomina el colágeno de tipo III, que proporciona un soporte estructural temporal pero carece de la resistencia del tejido maduro. La fase de remodelación (de 21 días a más de 6 meses) se caracteriza por la maduración del colágeno, la formación de enlaces cruzados y la reorganización del tejido a lo largo de las líneas de tensión mecánica. Las lesiones de grado I suelen curarse en 2-6 semanas, las de grado II en 6-12 semanas y las de grado III en 3-6 meses o más.
¿Qué es la crioterapia de CO₂?
Comprender la tecnología y los mecanismos que subyacen a la crioterapia con CO₂ es esencial para evaluar su potencial terapéutico en el tratamiento de distensiones y esguinces. Esta sección explora los fundamentos científicos y las aplicaciones prácticas de esta innovadora modalidad de tratamiento.
¿Qué es la crioterapia de CO₂? Definición y beneficios
La crioterapia con CO₂ es una técnica terapéutica avanzada que utiliza gas de dióxido de carbono a presión para proporcionar un enfriamiento controlado y localizado a temperaturas extremadamente bajas que alcanzan los -78 °C (-108 °F). El tratamiento aplica ráfagas controladas de dióxido de carbono directamente en las zonas afectadas, creando un choque térmico rápido mediante la administración de gas a presión que desencadena una vasoconstricción inmediata y reduce la demanda metabólica en los tejidos tratados. A diferencia de los métodos tradicionales de crioterapia, la crioterapia con CO₂ proporciona un control preciso de la temperatura y una aplicación selectiva, lo que permite a los profesionales personalizar los parámetros de tratamiento en función de las características específicas de la lesión y las necesidades del paciente. El sistema funciona mediante dispositivos de administración especializados que regulan la presión, la temperatura y la duración de la aplicación para optimizar los resultados terapéuticos. Las sesiones de tratamiento suelen durar entre 10 y 15 segundos por zona de aplicación, y el frío extremo genera respuestas fisiológicas inmediatas, como el alivio del dolor, la reducción de la inflamación y la mejora de la circulación. La precisión y la intensidad de la crioterapia con CO₂ permiten obtener efectos terapéuticos más específicos que con las aplicaciones de hielo convencionales.
En qué se diferencia la crioterapia de CO₂ de las bolsas de hielo y la crioterapia de cuerpo entero
Las diferencias fundamentales entre la crioterapia con CO₂ y los métodos de enfriamiento tradicionales radican en la precisión de la temperatura, el control de la aplicación y la profundidad de penetración terapéutica. Las bolsas de hielo convencionales suelen alcanzar temperaturas de entre 0 y 10 °C y requieren entre 15 y 20 minutos de aplicación para lograr efectos terapéuticos, lo que a menudo provoca irritación cutánea y patrones de enfriamiento desiguales. La crioterapia con CO₂ produce un choque térmico rápido a -78 °C, lo que provoca una vasoconstricción inmediata seguida de una vasodilatación reactiva que acelera el aporte de oxígeno y nutrientes a los tejidos dañados. Las cámaras de crioterapia de cuerpo entero exponen todo el cuerpo a temperaturas de entre -110 °C y -140 °C durante 2-4 minutos, lo que produce efectos sistémicos pero carece de la precisión necesaria para el tratamiento de lesiones específicas. La crioterapia de CO₂ combina la intensidad del frío extremo con la precisión localizada, lo que permite a los profesionales tratar estructuras anatómicas específicas sin afectar al tejido sano circundante. La duración controlada de la aplicación previene el daño tisular al tiempo que maximiza los beneficios terapéuticos mediante la activación óptima de la respuesta fisiológica.
Mecanismo de acción: Frío extremo, vasoconstricción y vasodilatación
Los mecanismos terapéuticos de la crioterapia con CO₂ se basan en respuestas fisiológicas al frío extremo que favorecen la curación de los tejidos y el alivio del dolor. La exposición al CO₂ induce rápidamente la vasoconstricción, reduciendo el flujo sanguíneo, la demanda metabólica y el daño secundario de los procesos inflamatorios. El enfriamiento repentino activa los termorreceptores y los nociceptores, desencadenando respuestas neurológicas que alivian el dolor a través de la teoría de la puerta de control. Tras la vasoconstricción inicial, se produce una vasodilatación reactiva que produce un "efecto de bombeo" que aumenta la circulación, mejora el aporte de nutrientes y acelera la eliminación de productos de desecho. Esta respuesta vascular alternante crea condiciones favorables para la reparación tisular. Además, la exposición al frío reduce la actividad de los mediadores inflamatorios y la función de las enzimas metabólicas, limitando el daño hipóxico a los tejidos sanos circundantes. Al reducir el consumo de oxígeno y modular el metabolismo celular, la crioterapia con CO₂ protege los tejidos lesionados durante las primeras fases críticas de la cicatrización. En conjunto, estos mecanismos explican su eficacia para reducir el dolor, controlar la inflamación y favorecer la recuperación de las lesiones musculoesqueléticas.
Cómo ayuda la crioterapia con CO₂ en distensiones y esguinces
Los beneficios terapéuticos de la crioterapia con CO₂ para distensiones y esguinces se derivan de su capacidad para abordar simultáneamente múltiples aspectos de la fisiopatología de la lesión. La comprensión de estos mecanismos ayuda a explicar por qué este tratamiento resulta prometedor para acelerar la recuperación.
Reducción de la inflamación y la hinchazón en el lugar de la lesión
La crioterapia de CO₂ reduce la inflamación y la hinchazón actuando sobre los mecanismos vasculares y celulares de la respuesta inflamatoria. El frío extremo desencadena una vasoconstricción inmediata de los vasos sanguíneos y linfáticos, lo que limita la fuga de fluidos y evita el edema excesivo en el lugar de la lesión. Este efecto vascular también restringe la acumulación de mediadores inflamatorios y células inmunitarias que intensifican el dolor y el daño tisular. A nivel celular, la crioterapia modula la actividad de las citocinas reduciendo los marcadores proinflamatorios como el TNF-α y la IL-1β y potenciando las respuestas antiinflamatorias. El proceso de enfriamiento reduce la demanda metabólica, disminuyendo el consumo de oxígeno y minimizando las lesiones hipóxicas secundarias en los tejidos sanos circundantes. Además, estabiliza la permeabilidad de la membrana y la función de los canales iónicos, reduciendo la inflamación celular y preservando la integridad estructural. Además, el rápido cambio de temperatura activa las respuestas termorreguladoras que favorecen la cascada de curación, creando un entorno que controla la inflamación perjudicial al tiempo que favorece la reparación y recuperación de los tejidos.
Alivio del dolor mediante la desensibilización neural
Los efectos analgésicos de la crioterapia con CO₂ son el resultado de sofisticadas interacciones con los mecanismos de procesamiento del dolor del sistema nervioso periférico y central. La aplicación de frío extremo afecta directamente a la función de los nociceptores a través de canales iónicos sensibles a la temperatura, en particular los canales TRPM8 (receptor 1 del frío y el mentol) y TRPA1 (receptor potencial transitorio anquirina 1) que modulan la transmisión de la señal del dolor. El rápido cambio de temperatura crea una fuerte entrada sensorial que activa las fibras nerviosas A-β de gran diámetro, las cuales, según la teoría de la puerta de control, inhiben las fibras C más pequeñas que transmiten el dolor a nivel de la médula espinal. Los cambios en la velocidad de conducción nerviosa inducidos por el frío reducen la velocidad e intensidad de la transmisión de la señal de dolor al cerebro, lo que proporciona un alivio inmediato. El tratamiento también desencadena la liberación de opioides endógenos, como endorfinas y encefalinas, que proporcionan analgesia mediada centralmente. Los efectos anestésicos locales se producen a través de la estabilización directa de la membrana neural y la reducción de la excitabilidad nerviosa. Estos mecanismos combinados crean un alivio inmediato y sostenido del dolor que facilita la movilización temprana y la recuperación funcional.
Mejora de la circulación y el suministro de oxígeno para una curación más rápida
La crioterapia con CO₂ mejora la circulación para crear las condiciones óptimas para la curación de los tejidos al mejorar la perfusión y el aporte de nutrientes. La alternancia de vasoconstricción y vasodilatación genera un efecto de "bombeo" que impulsa un flujo sanguíneo más eficiente en comparación con las terapias de frío estáticas. Este mecanismo aumenta el aporte de oxígeno, glucosa, aminoácidos y nutrientes esenciales para la reparación celular, al tiempo que acelera la eliminación de residuos metabólicos, restos inflamatorios y componentes tisulares dañados. La mejora de la circulación favorece la angiogénesis, permitiendo el crecimiento de nuevos vasos sanguíneos necesarios para mantener la perfusión en el tejido en regeneración. La crioterapia también estimula el drenaje linfático, reduciendo la congestión y eliminando el exceso de líquidos y mediadores inflamatorios. Al mejorar el tráfico de células inmunitarias, en particular la actividad de los macrófagos, la terapia acelera la eliminación del tejido dañado al tiempo que favorece la reparación y la regeneración. Juntos, estos efectos crean un entorno vascular y celular equilibrado que no sólo reduce la inflamación, sino que también favorece la recuperación funcional a largo plazo.
Apoyo a la reparación de tendones, ligamentos y tejidos musculares
La crioterapia de CO₂ ayuda a reparar las estructuras de los tejidos blandos mejorando el metabolismo celular, la síntesis de proteínas y la remodelación de los tejidos. El tratamiento estimula la actividad de los fibroblastos y la síntesis de colágeno, restaurando la integridad estructural de tendones y ligamentos. El aumento de la producción de ATP proporciona la energía necesaria para la síntesis de proteínas, la división celular y los procesos de reparación. Las fibras de colágeno se organizan a lo largo de las líneas de tensión, mejorando la resistencia biomecánica de los tejidos en curación. En el músculo, la crioterapia activa las células satélite y favorece la regeneración de las miofibras, facilitando la recuperación de los elementos contráctiles dañados. La terapia regula la actividad de la metaloproteinasa de matriz (MMP), equilibrando la descomposición y la síntesis de tejido durante la remodelación. También ayuda a restaurar la función muscular reduciendo la fatiga neuromuscular, lo que permite un retorno más rápido a la actividad. Además, la liberación de factores de crecimiento y la activación de vías de señalización favorecen la reparación integral de los tejidos y la restauración funcional de tendones, ligamentos y músculos. En conjunto, estos efectos convierten a la crioterapia en una valiosa herramienta para acelerar la recuperación y reforzar la cicatrización de los tejidos blandos.
Pruebas clínicas y opiniones de expertos
La evaluación de la eficacia de la crioterapia de CO₂ requiere un análisis cuidadoso de las pruebas de investigación disponibles y de las perspectivas expertas de los profesionales de la medicina deportiva. En esta sección se examina el estado actual del apoyo científico a este enfoque terapéutico.
Principales estudios de investigación sobre la crioterapia para lesiones deportivas
La investigación clínica sobre la crioterapia para lesiones deportivas muestra tanto beneficios como limitaciones. La mayoría de los estudios informan de efectos positivos en la reducción del dolor y la recuperación a corto plazo, pero muchos ensayos presentan deficiencias metodológicas que limitan las conclusiones sólidas. Las pruebas actuales no confirman que la crioterapia prevenga el daño tisular secundario o promueva directamente la regeneración tisular, a pesar de sus claros efectos analgésicos. Por ejemplo, los estudios indican que el tratamiento tradicional con hielo y compresión puede no proporcionar ventajas significativas sobre la no crioterapia en los esguinces de tobillo al medir el dolor, la inflamación y la amplitud de movimiento. Las revisiones sistemáticas destacan que la duración del tratamiento y la coherencia del protocolo son factores clave que influyen en los resultados, aunque éstos varían mucho de un estudio a otro. En cambio, las investigaciones más recientes sobre la crioterapia con CO₂ han arrojado resultados más prometedores. Los estudios demuestran que los métodos basados en el CO₂ pueden mejorar la circulación, acelerar la recuperación de la función muscular y proporcionar beneficios más constantes que las aplicaciones tradicionales de hielo, por lo que se están convirtiendo en un tema de interés creciente en la medicina deportiva.
Pruebas que apoyan la crioterapia de CO₂ para acelerar la recuperación
Las nuevas investigaciones destacan las ventajas de la crioterapia con CO₂ sobre los métodos tradicionales de enfriamiento para la recuperación de lesiones y la mejora del rendimiento. Los estudios clínicos han demostrado que la crioterapia con CO₂ proporciona mayores mejoras en la reducción del dolor, la capacidad funcional y los tiempos de vuelta a la actividad en comparación con la terapia de hielo estándar. La investigación también sugiere que el enfriamiento con CO₂ mejora la recuperación muscular inmediata de la fatiga neuromuscular, ofreciendo beneficios únicos para los atletas que buscan una restauración más rápida del rendimiento. Las aplicaciones localizadas de CO₂ se han relacionado con una reducción de los marcadores de inflamación, una mejora de la amplitud de movimiento de las articulaciones y una recuperación funcional más rápida en comparación con los tratamientos convencionales. Los resultados comunicados por los pacientes indican con frecuencia una mayor satisfacción y eficacia percibida con la crioterapia con CO₂. Las medidas objetivas, como la termografía, la ecografía y las pruebas biomecánicas, también demuestran respuestas superiores de curación de los tejidos con el tratamiento con CO₂. A pesar de estos resultados prometedores, la crioterapia con CO₂ sigue siendo una modalidad relativamente nueva, y se necesitan estudios a largo plazo con grandes poblaciones de pacientes para confirmar su eficacia y seguridad en medicina deportiva.
Cómo utilizan la crioterapia de CO₂ los médicos del deporte y los fisioterapeutas
Los profesionales de la medicina deportiva integran cada vez más la crioterapia con CO₂ en los protocolos de tratamiento de afecciones musculoesqueléticas agudas y crónicas. Los fisioterapeutas suelen combinar la crioterapia con CO₂ con la terapia manual, los programas de ejercicios y la educación del paciente para maximizar los resultados de la recuperación. Los médicos deportivos la recomiendan como intervención inmediata tras una lesión, sobre todo para los deportistas de competición que necesitan soluciones rápidas para volver a jugar. Más allá de la atención a las lesiones, la crioterapia con CO₂ también se utiliza en rutinas previas a la competición para mejorar la preparación muscular y en la recuperación posterior a la competición para reducir el dolor y acelerar la curación. Los médicos informan de resultados positivos en afecciones como distensiones musculares, esguinces de ligamentos, tendinopatías y lesiones por uso excesivo. Los protocolos habituales incluyen varias sesiones a lo largo de días o semanas, y la intensidad y frecuencia del tratamiento se ajustan a la gravedad de la lesión y a la respuesta del paciente. Muchos profesionales mejoran los resultados combinando la crioterapia de CO₂ con modalidades complementarias como la terapia de compresión, la estimulación eléctrica y los ultrasonidos terapéuticos, creando un enfoque sinérgico que favorece una recuperación musculoesquelética más rápida y completa.
Limitaciones y áreas que requieren más investigación
A pesar de los alentadores resultados iniciales, la investigación sobre la crioterapia con CO₂ sigue siendo limitada y requiere una investigación más sólida. Las pruebas científicas actuales son en gran medida anecdóticas debido a la escasez de ensayos controlados aleatorizados, una laguna que se extiende específicamente a las aplicaciones de crioterapia con CO₂. La estandarización de los protocolos de tratamiento -incluida la temperatura ideal, la duración, la frecuencia y el momento- aún no se ha establecido y debe abordarse en futuros estudios. La seguridad a largo plazo y los posibles efectos adversos siguen sin explorarse, sobre todo en caso de uso repetido o en poblaciones vulnerables. Aunque los mecanismos de acción propuestos son teóricamente sólidos, es necesario validarlos mediante investigaciones de laboratorio y ensayos clínicos que utilicen medidas objetivas de los resultados. También son necesarias comparaciones coste-eficacia con las terapias convencionales para fundamentar la toma de decisiones sanitarias y las políticas de seguros. La investigación futura debe centrarse en identificar los criterios óptimos de selección de pacientes, las contraindicaciones y los factores predictivos de la respuesta al tratamiento. En última instancia, los ensayos controlados aleatorizados multicéntricos a gran escala con un seguimiento prolongado son esenciales para desarrollar directrices clínicas basadas en la evidencia.
Quién puede (y quién no) beneficiarse de la crioterapia de CO₂?
Conocer la selección adecuada de pacientes para la crioterapia con CO₂ es crucial para optimizar los resultados del tratamiento y garantizar la seguridad del paciente. En esta sección se describen los candidatos ideales y las contraindicaciones importantes para este abordaje terapéutico.
Candidatos ideales (deportistas, adultos activos, casos crónicos)
- Los deportistas de élite y aficionados se benefician de una recuperación más rápida y de un alivio del dolor que favorece la constancia en el entrenamiento y la competición.
- Los adultos activos que practican deportes, hacen ejercicio o tienen ocupaciones exigentes pueden utilizar la crioterapia para tratar lesiones agudas y prevenir problemas crónicos.
- Las personas con dolores crónicos, como torceduras recurrentes o molestias articulares persistentes, pueden encontrar un alivio significativo.
- Los pacientes que no responden a tratamientos convencionales como la terapia con hielo, la medicación o la fisioterapia pueden mejorar con la crioterapia de CO₂.
- Quienes buscan opciones de tratamiento del dolor no invasivas y sin fármacos aprecian sus mínimos efectos secundarios y su perfil de seguridad.
Contraindicaciones (quién debe evitar el tratamiento)
- Las personas con alergia al frío, crioglobulinemia o urticaria por frío corren el riesgo de sufrir reacciones alérgicas graves.
- Los pacientes con trastornos circulatorios como la enfermedad vascular periférica o el fenómeno de Raynaud se enfrentan a riesgos de daño tisular.
- Las mujeres embarazadas deben evitar la crioterapia con CO₂ debido a los efectos desconocidos sobre la salud materna y fetal.
- Las heridas abiertas, las infecciones o la piel comprometida aumentan el riesgo de empeoramiento de la lesión o la infección.
- Las personas con enfermedades cardiovasculares graves, hipertensión no controlada o eventos cardiacos recientes pueden sufrir respuestas de estrés perjudiciales.
- Los pacientes con neuropatía o sensibilidad reducida no pueden detectar con seguridad las lesiones relacionadas con el frío.
Cuándo puede no ser la mejor opción
- Las lesiones agudas en las primeras 24-48 horas pueden beneficiarse más de un enfriamiento suave y reposo que de una crioterapia intensa con CO₂.
- Los desgarros graves de ligamentos, las roturas de tendones o las fracturas que requieran una reparación quirúrgica deben tratarse primero con las intervenciones médicas adecuadas.
- Los pacientes con baja tolerancia al frío extremo, incluidos aquellos con ansiedad o malestar por la crioterapia, pueden preferir tratamientos alternativos.
- Las personas que esperan resultados inmediatos pueden sentirse decepcionadas, ya que los beneficios suelen producirse gradualmente a lo largo de varios tratamientos.

Cuidados postratamiento y consejos para la recuperación
La optimización de los resultados de la crioterapia de CO₂ requiere una atención postratamiento integral y una planificación estratégica de la recuperación. Esta sección ofrece recomendaciones basadas en la evidencia para maximizar los beneficios terapéuticos y apoyar el proceso de curación.
Estiramientos suaves y movilidad después de la crioterapia
El trabajo de movilidad posterior a la crioterapia debe comenzar inmediatamente una vez que el dolor disminuye y mejora la flexibilidad de los tejidos. Los ejercicios suaves de amplitud de movimiento mantienen la movilidad articular y evitan la rigidez tras una lesión y la exposición al frío. Los estiramientos deben ser progresivos, haciendo hincapié en los movimientos sin dolor y evitando técnicas que tensionen los tejidos en curación. Realizar calentamientos dinámicos antes de los estiramientos ayuda a restablecer la temperatura de los tejidos y prepara los músculos para la actividad. Los ejercicios propioceptivos que ponen a prueba el equilibrio y la coordinación ayudan a restablecer el control neuromuscular y reducen el riesgo de volver a lesionarse. Dar prioridad a la calidad del movimiento frente a la cantidad garantiza una biomecánica y unos patrones motores adecuados. Los pacientes deben controlar su respuesta, ajustando la intensidad en función de la comodidad y los síntomas. Los efectos analgésicos de la crioterapia con CO₂ proporcionan una ventana óptima para el ejercicio terapéutico, que debe utilizarse estratégicamente para maximizar los beneficios de la recuperación.
Nutrición e hidratación para favorecer la cicatrización de los tejidos
Una nutrición e hidratación óptimas son esenciales para favorecer la reparación tisular tras la crioterapia de CO₂. Una ingesta adecuada de proteínas (1,2-2,0 g/kg de peso corporal) proporciona los aminoácidos necesarios para la síntesis de colágeno y la reparación muscular, especialmente durante la fase proliferativa de cicatrización. Los nutrientes antiinflamatorios -ácidos grasos omega-3, vitaminas D y C y polifenoles- ayudan a regular la inflamación y favorecen la regeneración tisular. Una hidratación adecuada favorece la función celular, la circulación, el transporte de nutrientes y la eliminación de residuos. Programar las comidas en torno al tratamiento, en particular las ricas en antioxidantes después de la sesión, puede mejorar la recuperación. Los micronutrientes clave, como el zinc, el cobre y la vitamina A, desempeñan funciones específicas en la cicatrización de heridas y la formación de colágeno y deben mantenerse en niveles óptimos. Evitar los alimentos o sustancias proinflamatorias, como el exceso de alcohol y los alimentos procesados, favorece aún más la recuperación. Las estrategias nutricionales individuales deben adaptarse a la gravedad de la lesión, el nivel de actividad y las demandas metabólicas para maximizar los beneficios terapéuticos de la crioterapia.
Descanso frente a recuperación activa: encontrar el equilibrio
El equilibrio entre reposo y actividad después de la crioterapia de CO₂ depende de la gravedad de la lesión, la fase de curación y la tolerancia individual. El reposo absoluto puede ser necesario inmediatamente después de lesiones graves para evitar daños mayores y permitir la curación inicial. Sin embargo, la movilización suave temprana suele dar mejores resultados que la inmovilización prolongada para la mayoría de las distensiones y esguinces, especialmente cuando el dolor se controla con crioterapia. La recuperación activa, que incluye actividad aeróbica ligera, movimientos suaves y ejercicios terapéuticos, favorece la circulación, previene el desacondicionamiento y ayuda a la curación. La progresión de la actividad debe guiarse por el dolor, teniendo en cuenta que los efectos analgésicos de la crioterapia pueden enmascarar los síntomas. La calidad y duración del sueño (7-9 horas) son fundamentales para la reparación de los tejidos y la resolución de la inflamación. La reincorporación gradual a las actividades normales en función de los hitos funcionales y no sólo del tiempo reduce el riesgo de nueva lesión. La orientación profesional garantiza que el equilibrio entre descanso y actividad se adapte a las circunstancias individuales, optimizando la recuperación y los resultados a largo plazo.
Combinar la crioterapia con ejercicios de rehabilitación
La integración de la crioterapia de CO₂ en los programas de ejercicios de rehabilitación mejora los resultados generales de la recuperación. La crioterapia previa al ejercicio reduce el dolor y la rigidez muscular, lo que permite realizar ejercicios terapéuticos más eficaces y mejorar la calidad del movimiento. La crioterapia posterior al ejercicio ayuda a controlar la inflamación y el dolor provocados por la carga de los tejidos durante la rehabilitación. Los protocolos de carga progresiva deben poner a prueba gradualmente los tejidos en curación mientras se utiliza la crioterapia para controlar los síntomas y favorecer la recuperación. El entrenamiento del movimiento funcional junto con la crioterapia restablece los patrones específicos del deporte o la actividad necesarios para la plena participación. El entrenamiento de fuerza debe progresar sistemáticamente, y la crioterapia debe ayudar a la adaptación y recuperación de los tejidos entre sesiones. Los ejercicios propioceptivos y de control neuromuscular se benefician de la reducción del dolor y el aumento de la movilidad que proporciona la crioterapia. La optimización del momento y la secuencia del tratamiento maximiza la ventana terapéutica creada por los efectos analgésicos y antiinflamatorios de la crioterapia, favoreciendo una rehabilitación eficaz y reduciendo el riesgo de nueva lesión.
Veredicto final: ¿Puede la crioterapia con CO₂ acelerar realmente la curación?
La crioterapia de CO₂ resulta muy prometedora para el tratamiento de distensiones y esguinces, aunque las pruebas definitivas de una curación acelerada requieren más investigación. El alivio inmediato del dolor, la reducción de la inflamación y el aumento de la circulación crean unas condiciones favorables para la reparación de los tejidos, lo que puede contribuir a una recuperación más rápida. Los estudios clínicos informan de efectos positivos en la reducción del dolor y la recuperación neuromuscular, con pruebas emergentes que sugieren que la crioterapia con CO₂ puede ofrecer ventajas sobre los métodos de enfriamiento tradicionales. Desde el punto de vista fisiológico, sus mecanismos -vasoconstricción seguida de vasodilatación reactiva, reducción de la demanda metabólica y mejora de la administración de nutrientes- proporcionan una sólida base teórica para sus efectos terapéuticos. El rápido choque térmico y la mejora de la circulación crean las condiciones óptimas para la curación de los tejidos. Sin embargo, la investigación se ve limitada por la escasez de ensayos aleatorizados de alta calidad y las pruebas en gran medida anecdóticas, lo que deja la seguridad a largo plazo y la estandarización de protocolos como áreas de estudio para el futuro. Para los pacientes que buscan opciones no invasivas y sin fármacos, la crioterapia con CO₂ es un complemento prometedor a la rehabilitación. Es probable que acelere el alivio del dolor y la recuperación funcional temprana, mejorando los resultados de los pacientes al tiempo que mantiene un excelente perfil de seguridad.



