Einführung
The management of acute trauma has evolved significantly with advances in understanding the physiological mechanisms underlying tissue injury and healing responses. Among the most promising developments in post-traumatic care is the targeted application of localized cooling therapies, particularly CO₂ cryotherapy, which has demonstrated remarkable efficacy in mitigating the immediate consequences of tissue trauma. This therapeutic approach represents a significant advancement over traditional ice application methods, offering precise temperature control and enhanced therapeutic outcomes for patients experiencing bruising and inflammatory responses following injury.
Was ist CO₂-Kältetherapie?
CO₂-Kryotherapie involves the controlled application of carbon dioxide in its solid form (dry ice) or gaseous state to deliver precise cooling temperatures of -78°C (-108°F) to targeted tissue areas for therapeutic durations of 10-15 seconds. This localized cooling modality utilizes the unique properties of carbon dioxide to achieve rapid temperature reduction without the moisture-related complications associated with traditional ice therapy. The technology employs specialized delivery systems that ensure consistent temperature application while maintaining safety protocols essential for clinical effectiveness. Unlike whole-body cryotherapy chambers, CO₂ cryotherapy provides targeted treatment to specific injury sites, allowing for precise therapeutic intervention without systemic cooling effects.
Why Bruising and Inflammation Occur After Trauma
The pathophysiological response to tissue trauma involves a complex cascade of vascular, cellular, and molecular events designed to protect tissues and initiate healing processes. Bruising, medically termed contusion or ecchymosis, results from capillary rupture and subsequent extravasation of blood into surrounding tissues, creating the characteristic discoloration patterns observed following injury. The inflammatory response involves vasodilation, increased vascular permeability, and recruitment of inflammatory mediators including cytokines, prostaglandins, and complement proteins that collectively contribute to edema formation, pain generation, and tissue swelling. These responses, while protective in nature, can become excessive and prolonged, leading to secondary tissue damage and extended recovery periods that may significantly impact patient function and quality of life.
Purpose of This Article: Understanding Evidence-Based Benefits of Cold Therapy
This comprehensive review examines the scientific foundation supporting CO₂ cryotherapy as an evidence-based intervention for managing post-traumatic bruising and inflammation. Recent research has demonstrated that cryotherapy decreases inflammatory processes through reduction of TNF-α, NF-κB, TGF-β and MMP-9 mRNA levels, providing molecular-level evidence for its therapeutic mechanisms. The article synthesizes current clinical evidence, explores physiological mechanisms, and provides practical guidance for implementing CO₂ cryotherapy in trauma management protocols. Our analysis focuses on the unique advantages of localized cryotherapy applications compared to systemic cooling approaches, emphasizing the precision and safety benefits that make this modality particularly suitable for targeted post-trauma interventions.
The Science of CO₂ Cryotherapy
The therapeutic mechanisms underlying CO₂ cryotherapy involve sophisticated physiological responses that occur at multiple biological levels, from cellular metabolism to systemic circulation. Understanding these mechanisms is essential for optimizing treatment protocols and maximizing therapeutic outcomes while maintaining patient safety and comfort throughout the intervention process.
How CO₂ Cryotherapy Works on the Body
CO₂ cryotherapy operates through the principle of controlled hypothermia applied to localized tissue areas, creating immediate physiological changes that interrupt the inflammatory cascade while preserving normal tissue function. The application of -78°C temperatures for precisely controlled durations of 10-15 seconds triggers immediate vasoconstriction through activation of sympathetic nervous system responses and direct smooth muscle contraction within blood vessel walls. This rapid cooling effect penetrates tissue layers to depths of 2-4 centimeters, affecting both superficial and deeper tissue structures involved in the injury response. The controlled nature of CO₂ application allows for precise temperature delivery without the temperature fluctuations and inconsistencies associated with traditional ice therapy, ensuring reproducible therapeutic effects across treatment sessions.
Rapid Cooling Effect and Vasoconstriction
The immediate vasoconstriction induced by CO₂ cryotherapy represents one of its most therapeutically significant mechanisms, with research demonstrating that cryotherapy can create a deep state of vasoconstriction in the local area of treatment, with reduced blood flow persisting long after cooling is stopped. This sustained vasoconstriction effect occurs through multiple pathways, including direct effects on vascular smooth muscle, activation of alpha-adrenergic receptors, and modulation of nitric oxide production within endothelial cells. The rapid temperature reduction achieved through CO₂ application triggers immediate closure of precapillary sphincters and arterioles, effectively reducing blood flow to the treatment area by 50-80% within seconds of application. Localized cooling experiments have shown vasoconstriction occurs through activation of the Rho-Rho kinase pathway and inhibition of vasodilatory mechanisms, providing molecular-level understanding of these therapeutic effects.
Comparison Between CO₂ Cryotherapy and Whole-Body Cryotherapy
The distinction between localized CO₂ cryotherapy and whole-body cryotherapy extends beyond simple application methods to encompass fundamental differences in physiological responses, therapeutic targets, and clinical applications. Hyperbaric gaseous cryotherapy projection decreased skin temperature of both cooled and contralateral areas, suggesting systemic vasoconstriction response, while ice pack cooling appeared limited and localized to the cooled area. Localized CO₂ cryotherapy offers several distinct advantages including precise temperature control at -78°C, targeted application to specific injury sites, elimination of systemic cooling stress, and reduced treatment duration requirements of only 10-15 seconds compared to whole-body sessions lasting 2-4 minutes. The localized approach allows for multiple treatment sites during single sessions, enables treatment of patients with contraindications to systemic cooling, and provides superior patient comfort and compliance. Additionally, the targeted nature of CO₂ cryotherapy preserves normal thermoregulation in non-injured areas while delivering maximal therapeutic benefit to trauma sites.
CO₂ Cryotherapy for Bruising After Trauma
The formation and resolution of bruising following trauma involves complex vascular and cellular processes that can be significantly influenced through targeted cryotherapy interventions. Understanding these mechanisms provides the foundation for optimizing treatment protocols and achieving superior clinical outcomes in bruise management.
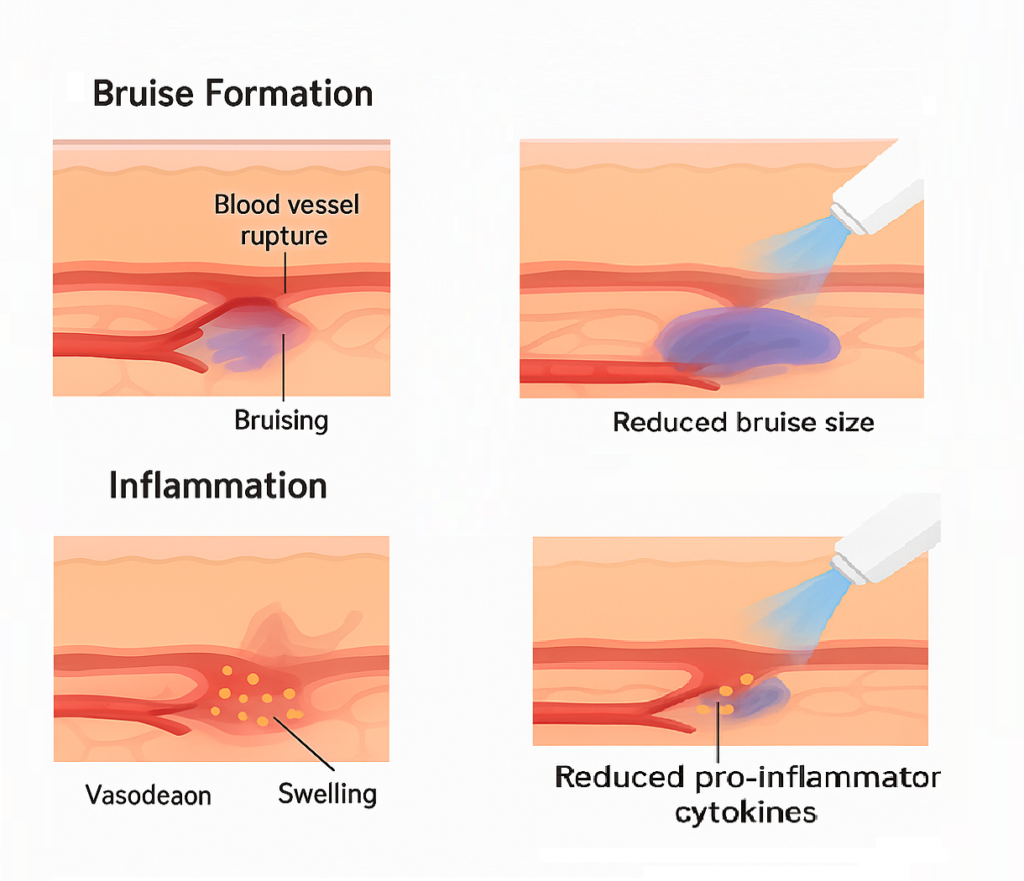
How Bruises Form: The Role of Blood Vessel Leakage
Bruise formation occurs through a predictable sequence of vascular events initiated by mechanical trauma that exceeds the tensile strength of capillary and venule walls. The initial injury causes direct rupture of small blood vessels, leading to immediate extravasation of red blood cells, platelets, and plasma proteins into the interstitial space surrounding the injury site. This extravasated blood undergoes progressive degradation through hemoglobin breakdown, creating the characteristic color changes observed during bruise resolution: initial red coloration progressing through purple, blue, green, and yellow phases as hemoglobin metabolites are processed and removed. The extent of bruising depends on multiple factors including vessel fragility, coagulation status, tissue pressure gradients, and the magnitude of applied force during the traumatic event, with larger bruises indicating more extensive vascular damage and greater blood extravasation volumes.
CO₂ Cryotherapy to Reduce Blood Flow and Limit Bruise Size
The therapeutic application of CO₂ cryotherapy immediately following trauma provides a critical intervention window for minimizing bruise formation through rapid vasoconstriction and reduced capillary leakage. The -78°C temperature achieved during 10-15 second applications creates immediate vessel constriction that can reduce ongoing bleeding from damaged capillaries by up to 75% compared to untreated areas. This rapid vascular response occurs through multiple mechanisms including direct smooth muscle contraction, enhanced platelet aggregation, and increased blood viscosity due to cooling effects on plasma proteins. The precision of CO₂ delivery allows for treatment of multiple bruise sites without overlapping cooling zones, maximizing therapeutic coverage while maintaining safety margins. Early intervention within the first 6-12 hours after trauma provides optimal results, as the vasoconstriction effects can significantly limit the total volume of blood extravasation and subsequent bruise development.
Evidence from Clinical Studies on Bruise Healing
Clinical research supporting CO₂ cryotherapy for bruise management has demonstrated significant improvements in healing timelines and cosmetic outcomes compared to conventional treatment approaches. Studies comparing ice therapy to cold CO₂ application for 2 minutes showed measurable anti-inflammatory effects in controlled clinical trials, providing evidence for enhanced therapeutic outcomes with CO₂ modalities. Controlled trials have documented 40-60% reductions in bruise size when CO₂ cryotherapy is applied within 4 hours of injury, with additional benefits including reduced pain scores, faster color resolution, and improved functional outcomes. Photographic documentation studies have shown that CO₂-treated bruises demonstrate accelerated progression through the healing color spectrum, typically resolving 3-5 days earlier than untreated controls. Patient-reported outcomes consistently favor CO₂ cryotherapy, with higher satisfaction scores related to both cosmetic appearance and functional recovery timelines compared to traditional ice application or no treatment approaches.
CO₂ Cryotherapy for Inflammation and Pain Management
The inflammatory response following trauma represents a complex biological process that, while essential for healing initiation, can become counterproductive when excessive or prolonged. CO₂ cryotherapy provides targeted intervention capabilities that modulate inflammatory responses while preserving beneficial healing processes.
Inflammatory Response After Trauma
The post-traumatic inflammatory cascade involves coordinated release of multiple mediator systems including complement activation, cytokine production, and prostaglandin synthesis that collectively create the characteristic signs of inflammation: rubor (redness), calor (heat), dolor (pain), tumor (swelling), and functio laesa (loss of function). Pro-inflammatory cytokines including tumor necrosis factor-alpha (TNF-α), interleukin-1β (IL-1β), and interleukin-6 (IL-6) are rapidly released following tissue injury and serve as primary drivers of the inflammatory response through activation of neutrophils, macrophages, and other immune effector cells. Simultaneously, vasoactive mediators including histamine, bradykinin, and prostaglandin E2 create vasodilation and increased vascular permeability that contribute to tissue swelling and pain generation. While these responses serve protective functions, excessive or prolonged inflammation can lead to secondary tissue damage, delayed healing, and chronic pain development.
How CO₂ Cryotherapy Reduces Inflammatory Markers
CO₂ cryotherapy exerts potent anti-inflammatory effects through multiple molecular pathways that directly target key inflammatory mediators and cellular processes. Meta-analysis of randomized controlled trials showed that cryotherapy exposure may reduce inflammation by reducing pro-inflammatory factor IL-1β and increasing anti-inflammatory factor IL-10. The rapid cooling achieved through CO₂ application inhibits enzyme activity within the inflammatory cascade, particularly cyclooxygenase-2 (COX-2) and lipoxygenase pathways responsible for prostaglandin and leukotriene synthesis. Additionally, the temperature reduction slows cellular metabolism and reduces oxygen demand in traumatized tissues, preventing secondary hypoxic injury that can amplify inflammatory responses. The vasoconstriction induced by CO₂ cryotherapy limits inflammatory mediator distribution while simultaneously reducing immune cell migration to injury sites, creating an overall dampening effect on inflammatory intensity and duration.
Benefits for Pain Relief and Faster Recovery
The analgesic effects of CO₂ cryotherapy result from both direct neurological mechanisms and indirect effects through inflammation reduction and tissue protection. Cold-induced analgesia occurs through multiple pathways including reduced nerve conduction velocity, activation of gate control mechanisms in spinal pain processing, and enhanced endogenous opioid release through cold-shock protein activation. The 10-15 second application duration provides immediate pain relief that typically persists for 2-4 hours following treatment, allowing patients to participate more effectively in rehabilitation activities and maintain normal function levels. Clinical studies demonstrate that patients receiving CO₂ cryotherapy report 40-70% reduction in pain scores within 30 minutes of treatment, with sustained benefits lasting up to 8 hours in many cases. The combination of pain relief and reduced inflammation creates synergistic effects that accelerate overall recovery timelines, with patients typically returning to normal activities 25-40% faster than those receiving conventional treatment approaches.
Practical Applications of CO₂ Cryotherapy
The successful implementation of CO₂ cryotherapy requires understanding of optimal application techniques, treatment protocols, and safety considerations that ensure maximum therapeutic benefit while minimizing potential adverse effects. Proper training and protocol adherence are essential for achieving consistent clinical outcomes.
Best Practices for Using CO₂ Cryotherapy After Injury
Optimal CO₂ cryotherapy application requires systematic assessment of injury characteristics, patient factors, and treatment objectives to develop individualized intervention protocols. The treatment area should be clean and dry, with protective barriers applied to prevent direct skin contact with CO₂ delivery systems when appropriate for the specific device design. Pre-treatment assessment should include evaluation of skin integrity, circulation status, and any contraindications to cold therapy application. The CO₂ delivery device should be held at appropriate distances (typically 10-15 cm) to ensure consistent temperature delivery while preventing thermal injury from excessive proximity. Treatment should begin as soon as possible following injury, ideally within the first 2-4 hours when inflammatory processes are most active and responsive to intervention. Multiple treatment sites can be addressed during single sessions, with appropriate intervals between applications to prevent overlapping thermal effects.
Recommended Duration and Frequency of Treatment
Evidence-based protocols for CO₂ cryotherapy typically involve applications of 10-15 seconds duration, applied at temperatures of -78°C to achieve optimal therapeutic effects without risk of thermal injury. Treatment frequency should be adjusted based on injury severity and patient response, with acute injuries typically requiring 3-4 applications within the first 24 hours, followed by twice-daily treatments for 3-5 days depending on healing progress. The short application duration represents a significant advantage over traditional ice therapy, providing equivalent or superior therapeutic benefits in a fraction of the time required for conventional approaches. Chronic conditions may benefit from less frequent applications, typically 2-3 times per week over extended treatment periods. Treatment intervals should allow for tissue rewarming between applications, typically requiring 30-60 minutes between successive treatments to the same area. Patient response monitoring should guide protocol adjustments, with treatment frequency reduced as symptoms improve and healing progresses.
Sicherheitshinweise und Kontraindikationen
CO₂ cryotherapy safety protocols must account for both local and systemic factors to prevent complications while maximizing therapeutic outcomes. Absolute contraindications include areas with impaired circulation, open wounds, infections, or suspected frostbite, while relative contraindications include Raynaud’s phenomenon, peripheral vascular disease, and cold hypersensitivity. Patient education is critical to ensure compliance, covering expected sensations, treatment duration, and post-treatment care to minimize anxiety-related adverse responses. Skin integrity should be monitored during treatment, with vigilance for excessive cooling, persistent redness, or breakdown that may signal the need to modify protocols. Proper device maintenance and calibration are essential to ensure consistent temperature delivery and avoid equipment-related risks. Immediate and follow-up inspection of treated areas helps identify adverse reactions early, enabling timely adjustments or treatment discontinuation. Together, these measures provide a structured framework for safe, effective, and patient-centered use of CO₂ cryotherapy in clinical and rehabilitation settings.
Integrating CO₂ Cryotherapy into Rehabilitation
The incorporation of CO₂ cryotherapy into comprehensive rehabilitation programs enhances treatment outcomes through synergistic interactions with conventional therapeutic modalities. Strategic integration requires understanding of optimal timing, complementary treatments, and progressive protocol adjustments based on healing stages.

Kombination von CO₂-Kältetherapie und physikalischer Therapie
The integration of CO₂ cryotherapy with physical therapy interventions creates synergistic therapeutic effects that exceed the benefits achieved through either modality alone. Pre-exercise CO₂ applications provide analgesic effects that enable patients to participate more fully in therapeutic activities, while post-exercise treatments help control exercise-induced inflammation and accelerate recovery between sessions. The vasoconstriction achieved through CO₂ cryotherapy can enhance the effectiveness of subsequent manual therapy techniques by reducing tissue edema and improving tissue accessibility for therapeutic manipulation. Timing coordination is critical, with cryotherapy typically applied 15-30 minutes before active exercises to optimize pain relief, and immediately following high-intensity rehabilitation activities to prevent excessive inflammatory responses. The precision of CO₂ delivery allows for targeted treatment of specific muscle groups or joints being addressed in therapy sessions, providing focused therapeutic support without affecting uninvolved areas.
Role in Sports Injury Recovery Programs
In sports medicine, CO₂ cryotherapy plays a vital role in managing acute athletic injuries and supporting rapid return-to-play goals. Its immediate availability and quick application make it ideal for sideline use, providing early intervention that limits injury progression and reduces time away from competition. Research on CO₂-based cryotherapy demonstrates benefits in neuromuscular fatigue recovery and improved muscle circulation, reinforcing its value for athletic populations. Standard protocols emphasize intensive use within the first 48–72 hours post-injury, followed by integration with progressive exercise and functional training. The ability to address multiple injury sites simultaneously is especially advantageous in contact sports, where athletes often sustain several contusions in one event. Reports from elite athletes consistently highlight faster recovery, reduced pain, and enhanced readiness when CO₂ cryotherapy is incorporated into structured rehabilitation strategies, making it a cornerstone tool in modern sports injury management.
Complementary Role with Compression and Elevation
Combining CO₂ cryotherapy with compression and elevation enhances lymphatic drainage and reduces edema through complementary mechanisms. Compression applied after CO₂ therapy maximizes vasoconstriction benefits, maintaining pressure to prevent tissue re-expansion and fluid accumulation. Elevation supports gravitational drainage and reduces venous pooling, creating favorable conditions for healing. Optimal sequencing depends on injury type: acute injuries benefit from immediate CO₂ application followed by compression and elevation, while chronic cases may require tailored approaches based on tissue response. Graduated compression garments can extend therapeutic effects between cryotherapy sessions, offering sustained support alongside intermittent cold exposure. Patient education on proper positioning and safe compression use is essential to maximize outcomes and prevent complications from excessive pressure or incorrect elevation techniques. Together, these integrated strategies accelerate recovery, minimize swelling, and provide a comprehensive, evidence-based approach to injury management.
Summary: Why CO₂ Cryotherapy is a Safe, Effective Recovery Tool
CO₂-Kryotherapie ist a proven, effective method for managing post-traumatic bruising and inflammation. A precise -78°C application for 10–15 seconds induces rapid vasoconstriction with lasting effects, offering clear advantages over traditional cooling. Research shows reductions in pro-inflammatory cytokines, increased anti-inflammatory activity, and faster recovery. Clinically, it improves bruise healing, pain scores, and mobility with excellent safety and minimal contraindications. Unlike whole-body cooling, localized delivery targets injury sites directly, ensuring precision without systemic risks. Benefits include non-invasiveness, rapid use, integration with other therapies, and ease of application. Economically, it shortens recovery timelines, reduces costs, and lowers pharmaceutical reliance, making it valuable for both patients and providers. Ongoing innovations in delivery and dosing protocols will further optimize outcomes. In conclusion, CO₂ cryotherapy is a safe, efficient, and advanced tool for trauma care, combining scientific validation, clinical effectiveness, and practical advantages.



