Einführung
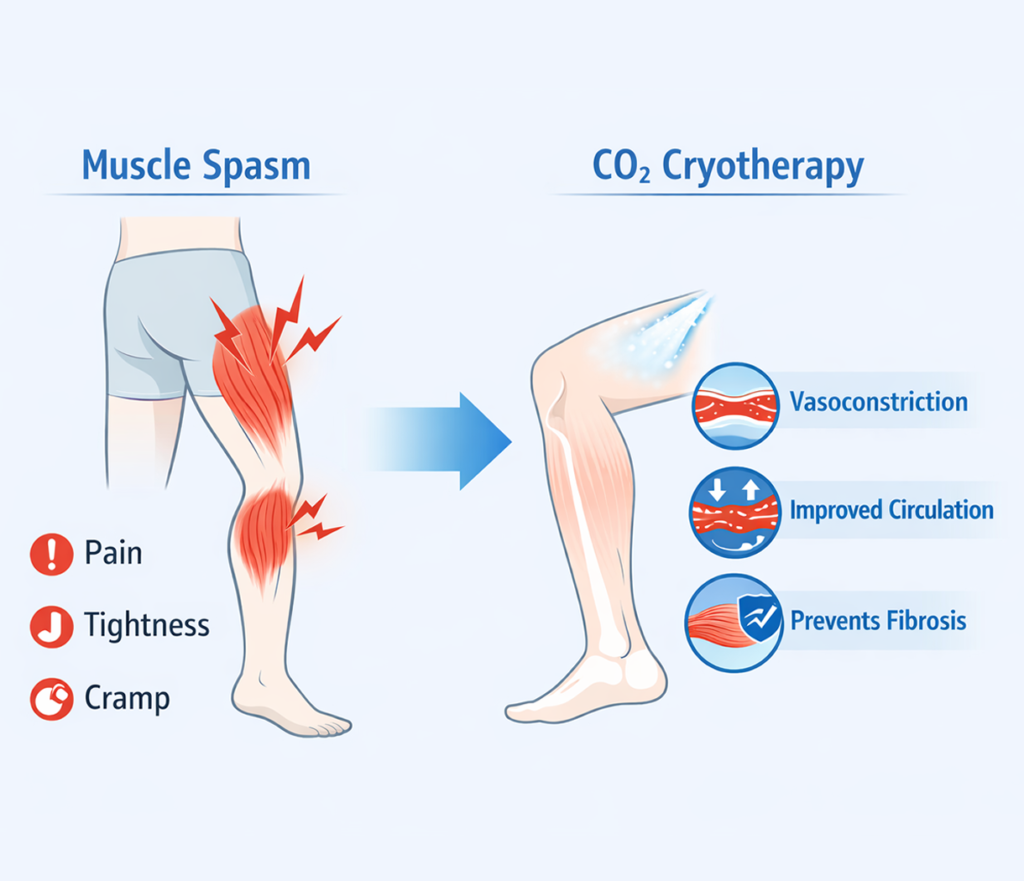
Muscle spasms and fibrosis are common issues that affect athletes, active individuals, and patients recovering from injuries. A muscle spasm is an involuntary contraction that can range from mild discomfort to severe pain, often limiting daily activities and athletic performance. When left untreated or when recurring frequently, these spasms can contribute to fibrosis—a process in which scar tissue forms within the muscle, decreasing flexibility, impairing function, and increasing susceptibility to re-injury. CO₂ cryotherapy has emerged as a non-invasive, drug-free therapy that may help manage muscle spasms, improve circulation, and reduce the risk of fibrosis. By applying controlled cold therapy to affected areas, CO₂ cryotherapy may modulate inflammatory responses, support cellular repair, and promote optimal muscle function. This article explores the physiological mechanisms, clinical applications, and benefits of CO₂ cryotherapy in preventing fibrosis and managing muscle spasms effectively.
1. Understanding Muscle Spasms and Fibrosis
Before delving into therapy, it is essential to understand the pathophysiology of muscle spasms and fibrosis. This understanding provides context for how cold therapy, such as CO₂ cryotherapy, can influence recovery and prevent long-term complications.
1.1 What Are Muscle Spasms?
Muscle spasms are involuntary contractions of skeletal muscle that can be caused by fatigue, electrolyte imbalances, nerve irritation, or trauma. They can occur acutely after intense physical activity or chronically due to repetitive strain or neurological conditions. Spasms may present as localized cramping or generalized tightness, often accompanied by pain, stiffness, and restricted range of motion. Persistent muscle spasms are not merely uncomfortable; they can interfere with normal tissue function and increase the risk of secondary injuries. Frequent contractions may induce microtears within the muscle fibers, perpetuating a cycle of inflammation, pain, and further spasm.
1.2 Fibrosis: When Muscle Heals Too Hard
Fibrosis occurs when the body responds to repeated microtrauma or chronic inflammation by depositing excess collagen within the muscle tissue. While collagen is essential for structural support, excessive or disorganized collagen can stiffen the muscle, reduce elasticity, and impair movement. This scar tissue formation is a natural part of the healing process but becomes problematic when it exceeds normal physiological levels. Muscle fibrosis is common after chronic spasms, prolonged immobilization, or severe injuries. It contributes to functional limitations, reduced athletic performance, and a higher likelihood of recurrent spasms. Preventing fibrosis is crucial to maintaining long-term muscle health.
2. Conventional Treatments and Their Limitations
Muscle spasms and fibrosis are typically managed with medications, physical therapy, or a combination of both. While these methods can provide symptom relief, they often have limitations that create a need for alternative therapies like CO₂ cryotherapy.
2.1 Medication and Muscle Relaxants
Pharmacologic treatments for spasms often include nonsteroidal anti-inflammatory drugs (NSAIDs) and muscle relaxants. NSAIDs work by inhibiting cyclooxygenase enzymes to reduce inflammation and pain, whereas muscle relaxants decrease involuntary contractions by modulating central or peripheral nervous system activity. While effective in the short term, these medications do not address the underlying tissue changes that lead to fibrosis. Long-term or frequent use may also lead to gastrointestinal irritation, renal impairment, sedation, or dependency. Consequently, medication alone is insufficient for long-term muscle health or fibrosis prevention.
2.2 Physical Therapy and Stretching
Physical therapy focuses on improving flexibility, strength, and neuromuscular coordination. Techniques may include targeted stretching, myofascial release, massage, and guided exercise programs. While these interventions are essential for rehabilitation, their effectiveness is limited if the underlying inflammation, microtrauma, or excessive collagen deposition is not addressed. Moreover, chronic or severe spasms may reduce the patient’s ability to participate fully in therapy, slowing recovery and potentially increasing the risk of fibrosis.
3. How CO₂ Cryotherapy Works on Muscles
CO₂ cryotherapy leverages controlled cold exposure to target muscle tissue, producing physiological effects that reduce spasms, support healing, and prevent fibrosis. The therapy’s mechanisms are multi-layered, involving vascular, cellular, and metabolic processes.
3.1 Mechanism: Vasoconstriction and Reactive Hyperemia
Upon exposure to CO₂ cold therapy, superficial blood vessels constrict (vasoconstriction), reducing local blood flow and limiting inflammation in the affected area. After removal of the cold stimulus, reactive hyperemia occurs, restoring blood flow with increased oxygen and nutrient delivery. This process helps flush metabolic waste, reduce localized swelling, and improve tissue oxygenation. For spasming muscles, these vascular effects help relax fibers, reduce ischemia-induced pain, and prepare the tissue for rehabilitation exercises. Reactive hyperemia also stimulates microcirculation, which is critical for tissue repair and scar tissue modulation.
3.2 Cellular Effects: Reducing Inflammation and Supporting Repair
At the cellular level, cold exposure modulates inflammatory mediators, decreasing levels of cytokines such as TNF-α and IL-6 that contribute to muscle irritation and fibrosis. CO₂ cryotherapy can enhance mitochondrial activity in skeletal muscle cells, increasing ATP production and supporting cellular repair. This metabolic boost accelerates the resolution of microtears, reduces oxidative stress, and promotes organized collagen deposition, mitigating the formation of excessive scar tissue. By influencing both inflammatory pathways and cellular metabolism, CO₂ cryotherapy addresses the root contributors to fibrosis while simultaneously alleviating muscle spasm.
4. Clinical Applications of CO₂ Cryotherapy
CO₂ cryotherapy has diverse clinical applications, from acute injury management to chronic muscle conditions. Its use extends across rehabilitation, sports medicine, and preventive care for high-risk individuals.
4.1 Acute Muscle Spasms
For acute injuries or sudden muscle cramps, CO₂ cryotherapy can be applied directly to the affected area to provide rapid analgesic effects. By reducing local inflammation and metabolic activity, it diminishes pain and muscle tension within minutes. This immediate relief not only improves comfort but also allows patients to engage in gentle movement or physical therapy sooner, preventing prolonged immobilization and secondary fibrosis. Clinical observations indicate that repeated, controlled sessions can enhance tissue recovery while minimizing the risk of long-term stiffness or scar formation.
4.2 Chronic Muscle Issues
Chronic muscle tightness, overuse injuries, and recurrent spasms are particularly prone to fibrosis. CO₂ cryotherapy, when used regularly as part of a rehabilitation program, helps manage ongoing inflammation and supports muscular relaxation. By improving circulation and nutrient delivery over repeated sessions, it reduces the cumulative microtrauma that can lead to fibrotic changes. Athletes, office workers, and patients with chronic musculoskeletal conditions often incorporate cold therapy alongside stretching and strengthening exercises to maintain flexibility and reduce recurrence of spasms.
4.3 Fibrosis Prevention
Preventing fibrosis is one of the most significant long-term benefits of CO₂ cryotherapy. By modulating inflammatory pathways and supporting organized tissue repair, cold therapy can influence collagen deposition, reducing the likelihood of excessive scar formation. This is particularly important for athletes recovering from intense training, patients post-injury, or individuals prone to repetitive strain injuries. Fibrosis prevention not only preserves muscle elasticity but also enhances performance, minimizes discomfort, and decreases the risk of re-injury over time.
5. Advantages of CO₂ Cryotherapy Over Traditional Methods
CO₂ cryotherapy offers several advantages compared to conventional treatments such as ice packs, medications, or passive rehabilitation.
5.1 Non-Invasive and Drug-Free
Unlike pharmacologic interventions, CO₂ cryotherapy does not require ingestion of medications or injections. This makes it suitable for individuals who cannot tolerate NSAIDs or muscle relaxants due to side effects or contraindications.
5.2 Safe for Repeated Use
The controlled application of CO₂ ensures a consistent and safe cooling effect without causing tissue damage or frostbite. Patients can receive multiple sessions in a week if needed, making it ideal for both acute and chronic conditions.
5.3 Can Be Combined with Physical Therapy and Exercise
Cold therapy complements other rehabilitation modalities. By reducing muscle tension and pain, it allows patients to engage more effectively in stretching, strengthening, and mobility exercises, thereby enhancing overall outcomes and preventing fibrosis.
6. Who Can Benefit From CO₂ Cryotherapy?
CO₂ cryotherapy is versatile and can benefit a wide range of individuals, from elite athletes to patients recovering from musculoskeletal injuries.
6.1 Athletes and Active Individuals
Athletes undergoing intensive training or participating in high-impact sports are prone to muscle spasms and micro-injuries. CO₂ cryotherapy can accelerate recovery, reduce the risk of fibrosis, and improve performance by maintaining muscle flexibility.
6.2 Patients Recovering from Injuries or Surgery
Post-injury and post-surgical patients benefit from CO₂ cryotherapy through reduced inflammation, improved circulation, and pain relief. These effects support early mobilization and prevent the formation of excessive scar tissue within muscles.
6.3 People with Chronic Muscle Pain or Spasms
Individuals with chronic conditions, such as myofascial pain syndrome or repeated strain injuries, can use CO₂ cryotherapy to manage discomfort, minimize flare-ups, and protect muscles from fibrosis over time.
FAQ
Can CO₂ Cryotherapy completely cure muscle spasms?
No, it is primarily a symptom management and preventative therapy. It helps reduce spasms, relieve pain, and prevent fibrosis but does not eliminate the underlying cause in all cases.
How long before I notice improvement?
Acute relief can be felt within minutes after a session, but chronic conditions may require multiple sessions over several weeks for optimal results.
Is CO₂ Cryotherapy safe for long-term use?
Yes, it is considered safe for repeated use under professional guidance. Sessions are non-invasive, and the therapy is drug-free.
Are there any safety considerations?
Patients should avoid direct exposure on open wounds or extremely sensitive skin areas. Sessions should be supervised by trained personnel.
Can it be combined with physical therapy or medications?
Yes, CO₂ cryotherapy complements physical therapy and can be used alongside medications for more comprehensive pain and muscle management.
Schlussfolgerung
Muscle spasms and fibrosis are common challenges that can compromise mobility, performance, and overall quality of life. CO₂ cryotherapy provides a non-invasive, drug-free solution to manage muscle spasms, support tissue repair, and prevent excessive scar formation. By leveraging physiological mechanisms such as vasoconstriction, reactive hyperemia, and cellular modulation, CO₂ cryotherapy addresses both symptoms and underlying tissue changes. Integrating cold therapy with rehabilitation exercises or recovery programs offers a powerful strategy for athletes, post-injury patients, and individuals with chronic muscle issues to maintain healthy muscle function, reduce pain, and prevent fibrosis effectively.
Referenzen
Low-Level Laser and Cryotherapy Mechanisms in Muscle Recovery:
https://pubmed.ncbi.nlm.nih.gov/16942950/
Muscle Spasms and Fibrosis: Pathophysiology and Management:
https://www.sciencedirect.com/science/article/abs/pii/S1047965110000117
CO₂ Cryotherapy in Sports Medicine and Injury Rehabilitation:


