Einführung
The therapeutic application of extreme cold has evolved significantly from simple ice pack applications to sophisticated delivery systems that harness the unique properties of carbon dioxide to create controlled, localized hypothermic conditions. Modern CO₂ cryotherapy represents a paradigm shift in how we understand and apply cold therapy, moving beyond symptom management to address fundamental physiological processes that govern tissue health and recovery. The growing body of research supporting CO₂ cryotherapy’s effects on microcirculation has revealed mechanisms that extend far beyond simple vasoconstriction and pain relief. These discoveries have positioned CO₂ cryotherapy as a valuable tool for enhancing microvascular function, optimizing tissue metabolism, and supporting natural healing processes through precisely controlled thermal stress.
Überblick über die CO₂-Kryotherapie
CO₂-Kryotherapie uses the rapid expansion and sublimation of liquid carbon dioxide to create extremely low temperatures (-78°C) for precise, targeted tissue therapy. Unlike ice, cold water, or air-based cryotherapy, CO₂ allows instantaneous temperature delivery with controlled exposure times, typically 10–15 seconds per site. Specialized devices safely apply CO₂ gas or snow to target areas, creating a temperature gradient exceeding 100°C, which triggers rapid physiological responses beyond the application site. Modern systems include automatic shut-off, temperature monitoring, and flow control, ensuring therapeutic benefit while minimizing tissue risk. The localized application allows focused treatment of specific regions without the cardiovascular stress of whole-body cryotherapy, making CO₂ cryotherapy a precise and efficient tool for enhancing recovery and promoting microcirculation.
Importance of Microcirculation in Health and Recovery
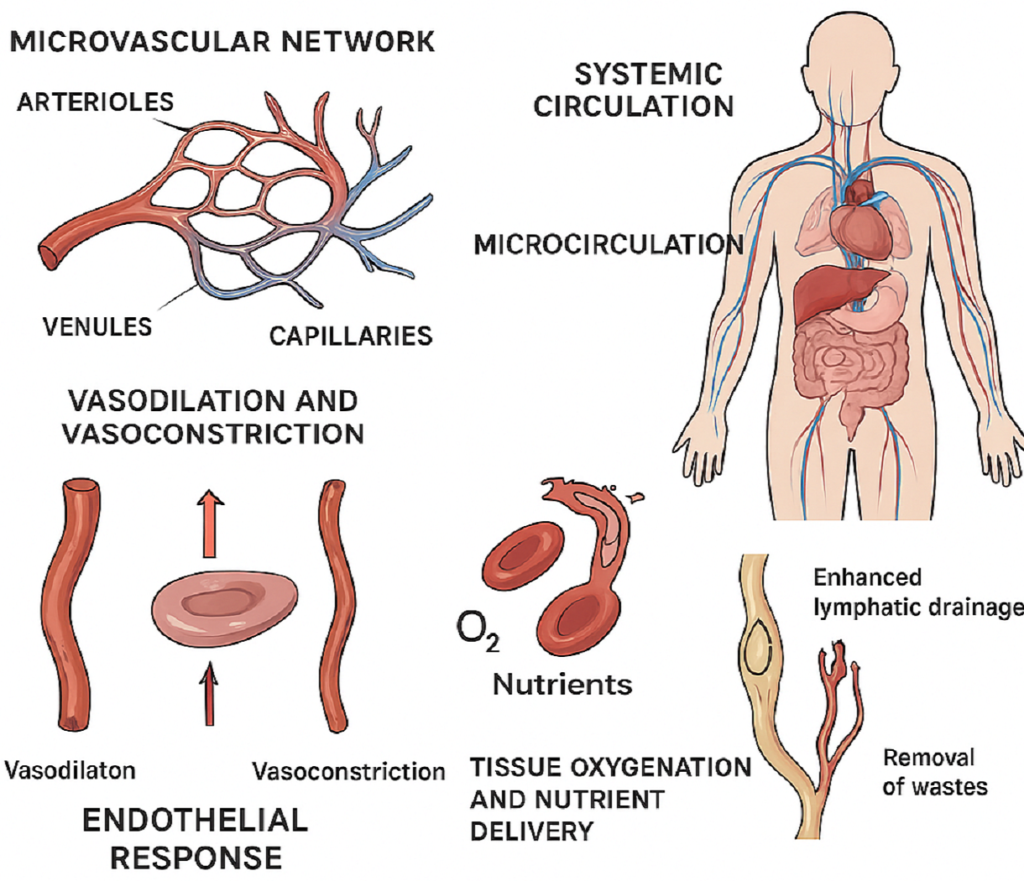
Microcirculation consists of arterioles, capillaries, and venules smaller than 100 micrometers, enabling oxygen, nutrient, and waste exchange between blood and tissues. It forms the functional interface where systemic circulation meets cellular metabolism, critical for tissue repair, health, and performance. Microvascular function adapts dynamically to physiological demands via endothelial regulation, smooth muscle tone, and neurogenic control. Dysfunction can lead to delayed healing, chronic pain, metabolic issues, and reduced athletic performance. Therapies that enhance microcirculation improve tissue perfusion, recovery, and overall function. CO₂ cryotherapy stimulates microvascular responses through controlled thermal stress, offering a non-invasive method to optimize circulation, particularly in areas where conventional treatments may be limited or unsuitable.
Purpose of the Article
This comprehensive analysis examines the physiological mechanisms through which CO₂ cryotherapy influences microcirculation, exploring the cellular and molecular processes that mediate therapeutic benefits observed in clinical and athletic applications. By understanding these underlying mechanisms, practitioners and patients can optimize treatment protocols, set appropriate expectations, and integrate CO₂ cryotherapy effectively within comprehensive therapeutic programs. The article synthesizes current research findings with clinical observations to provide evidence-based insights into optimal application parameters, expected outcomes, and safety considerations for CO₂ cryotherapy. Special attention is given to the unique properties of CO₂ as a therapeutic medium and how these characteristics translate into specific microcirculatory benefits that distinguish this approach from other cryotherapy modalities.
Verständnis der CO₂-Kryotherapie
The therapeutic application of carbon dioxide in cryotherapy represents a sophisticated approach to controlled hypothermic treatment that leverages the unique physical and chemical properties of CO₂ to create precise, localized therapeutic effects. Understanding the fundamental principles underlying CO₂ cryotherapy provides essential context for appreciating its specific effects on microcirculation and tissue physiology. The evolution of CO₂ cryotherapy from industrial cooling applications to medical therapeutics reflects advances in our understanding of controlled thermal stress and its effects on biological systems. This transition has been facilitated by technological developments that enable safe, precise delivery of therapeutic cold while monitoring and controlling exposure parameters to optimize benefit while minimizing risk.
Was ist CO₂-Kältetherapie?
CO₂ cryotherapy applies carbon dioxide in gas, liquid, or solid (dry ice) form to create controlled hypothermic conditions in target tissues. Sessions typically last 10–15 seconds, using CO₂ at -78°C, inducing rapid thermal transitions that trigger physiological responses beyond the immediate cooling effect. The therapy relies on CO₂’s phase transition properties, particularly sublimation from solid to gas, which absorbs heat and produces consistent cooling. Unlike ice-based methods, CO₂ delivers predictable, uniform temperatures for effective tissue therapy. Modern systems include precision delivery controls, monitoring flow rate, pressure, and exposure duration to ensure safety and optimal therapeutic effect. Automatic shutoff and temperature sensors prevent overexposure. The localized application allows targeted treatment of specific anatomical regions without systemic temperature changes, making CO₂ cryotherapy a precise and effective tool for enhancing microcirculation, tissue recovery, and pain modulation.
CO₂ Properties Relevant to Therapy
Carbon dioxide’s physical and chemical properties make it ideal for therapeutic cryotherapy. It is non-toxic, non-flammable, and naturally present in the body, eliminating chemical risks associated with other cooling agents. CO₂ is colorless and odorless, with visible vapor during application for clear treatment monitoring. High thermal conductivity enables rapid heat transfer, achieving therapeutic temperature differentials within seconds and minimizing exposure time while maximizing physiological response. Upon phase transition from liquid to gas, CO₂ expands, creating localized pressure and flow patterns that enhance tissue contact and even temperature distribution. These properties ensure consistent and predictable outcomes across different anatomical regions and patient populations. Rapid dissipation prevents prolonged tissue exposure, reducing risk while maintaining efficacy. CO₂’s unique dynamics combine efficiency, safety, and precision, making it superior to traditional cryotherapy methods for targeted microcirculation enhancement.
Safety and Tolerability
CO₂ cryotherapy is safe and well-tolerated when applied correctly. Short, localized sessions (10–15 seconds) minimize tissue risk while delivering sufficient thermal stress to trigger therapeutic responses, allowing frequent treatments without cumulative adverse effects. Its non-toxic nature eliminates chemical exposure concerns. CO₂ is rapidly expelled via normal respiration, leaving no residual effects, making it suitable for patients with chemical sensitivities or frequent therapy needs. Safety depends on proper application techniques, adherence to exposure parameters, and practitioner training. Devices with temperature monitoring and automatic shutoff ensure controlled delivery, while real-time feedback allows adjustments based on patient response. Overall, CO₂ cryotherapy combines efficacy with a strong safety profile, offering repeated, targeted treatment for microcirculation, recovery, and tissue health without systemic stress.
Microcirculation: The Physiological Foundation
Microcirculation represents the functional interface between systemic cardiovascular function and cellular metabolism, encompassing the intricate network of microscopic vessels that facilitate nutrient delivery, waste removal, and regulatory molecule exchange at the tissue level. Understanding microcirculatory physiology provides essential context for appreciating how CO₂ cryotherapy influences tissue health and recovery through vascular mechanisms. The complexity of microcirculatory regulation involves multiple overlapping control systems including myogenic, metabolic, neurogenic, and endothelial mechanisms that respond dynamically to local tissue demands and systemic conditions. This regulatory sophistication allows microcirculation to adapt rapidly to changing physiological conditions while maintaining optimal tissue perfusion under diverse circumstances.
Definition and Role of Microcirculation
Microcirculation comprises the smallest blood vessels—arterioles (10–100 μm), capillaries (5–10 μm), and venules (10–100 μm)—which facilitate exchange of oxygen, nutrients, hormones, and metabolic waste between blood and tissues. These vessels represent about 95% of the body’s vasculature and are the primary site where systemic circulation supports cellular metabolism. Arterioles regulate local blood flow, capillaries provide the main exchange surface, and venules aid waste removal and immune cell trafficking, creating an efficient network for dynamic tissue metabolic needs. Microcirculatory function is tightly regulated by smooth muscle tone, endothelial signaling, and neural control, responding to local metabolic demand, systemic cardiovascular status, and environmental changes. This allows rapid adaptation to tissue needs while maintaining optimal perfusion pressure and flow distribution, ensuring tissues receive consistent oxygen and nutrient supply, critical for health, recovery, and functional performance.
Microcirculation and Systemic Health
Healthy microcirculation is essential for overall physiological performance. Dysfunction contributes to conditions such as diabetes complications, cardiovascular disease, chronic pain, and impaired wound healing. Optimal microvascular function ensures efficient nutrient delivery, waste removal, and tissue homeostasis, supporting tissue repair and metabolism. Age and cardiovascular compromise can reduce capillary density, endothelial function, and autoregulation, increasing susceptibility to injury and slowing recovery. Interventions enhancing microcirculation—including exercise, nutrition, and therapeutic methods like CO₂ cryotherapy—can improve tissue health and overall quality of life. Monitoring microvascular function provides insights into therapeutic effectiveness and guides individualized treatment. Supporting microcirculation is thus a cornerstone for recovery, performance, and long-term systemic health, particularly in aging populations or those with compromised vascular function.
Measuring Microcirculation Changes
Microcirculatory function can be assessed using non-invasive technologies such as laser Doppler flowmetry, orthogonal polarization spectroscopy, and near-infrared spectroscopy. These methods evaluate blood flow, vessel density, and tissue oxygenation, offering objective data for therapy optimization. Laser Doppler flowmetry measures real-time microvascular perfusion by analyzing light scattering from red blood cells, making it valuable for evaluating immediate effects of CO₂ cryotherapy. Near-infrared spectroscopy assesses tissue oxygenation and hemoglobin saturation, revealing metabolic consequences of microcirculatory changes. These measurements help distinguish primary vascular effects from secondary metabolic benefits, enabling precise understanding of therapeutic mechanisms. By providing quantitative feedback, they allow clinicians to tailor treatment protocols, maximize efficacy, and monitor patient-specific responses, ensuring consistent microcirculation enhancement and recovery outcomes.
How CO₂ Cryotherapy Affects Microcirculation
The interaction between CO₂ cryotherapy and microcirculation involves complex physiological mechanisms that extend far beyond simple thermal effects. The extreme temperature differential created by CO₂ application initiates cascading responses throughout the microvascular network, influencing vessel tone, endothelial function, and tissue metabolism in ways that promote enhanced circulation and tissue health. Understanding these mechanisms provides insight into optimal treatment protocols and expected outcomes while explaining the sustained benefits often observed following CO₂ cryotherapy applications. The following sections explore the specific pathways through which controlled hypothermic stress translates into improved microcirculatory function and tissue health.
Vasodilation and Vasoconstriction Mechanisms
CO₂ cryotherapy triggers a biphasic vascular response: an initial vasoconstriction followed by reactive vasodilation. Immediate vasoconstriction, lasting 2–5 minutes, occurs via smooth muscle activation and sympathetic nervous system signaling, protecting tissues from extreme cold. The subsequent vasodilation phase is mediated by nitric oxide, prostaglandins, and metabolic vasodilators, enhancing microvascular perfusion. Blood flow can increase above baseline, improving nutrient delivery and waste removal. The extent and duration of vasodilation depend on tissue temperature, CO₂ exposure time, intensity, and individual vascular reactivity. Understanding these factors allows optimization of treatment protocols, maximizing therapeutic benefit while ensuring patient safety and comfort. This mechanism underpins CO₂ cryotherapy’s effectiveness for enhancing local circulation, accelerating recovery, and supporting tissue health.
Nitric Oxide Release and Endothelial Response
CO₂ cryotherapy stimulates endothelial nitric oxide synthase (eNOS), increasing nitric oxide (NO) production. NO acts as a vasodilator and anti-inflammatory mediator, promoting microvascular relaxation, improving blood flow, and reducing platelet aggregation. Endothelial responses include upregulation of heat shock proteins, antioxidants, and anti-inflammatory cytokines, supporting vascular health and resilience to stress. These adaptations improve flow-mediated vasodilation, barrier function, and reduce inflammatory marker expression, sustaining microcirculatory benefits beyond the treatment period. Enhanced endothelial function is particularly beneficial in conditions with endothelial dysfunction, such as diabetes, cardiovascular disease, and chronic inflammation. By improving microvascular health, CO₂ cryotherapy supports tissue perfusion, recovery, and overall vascular resilience.
Tissue Oxygenation and Nutrient Delivery Improvement
CO₂ cryotherapy enhances microcirculation, improving tissue oxygenation through increased capillary perfusion and reduced diffusion distance. Near-infrared spectroscopy shows sustained oxygen saturation increases for hours post-treatment. Improved blood flow also boosts nutrient delivery, including glucose, amino acids, and vitamins, supporting cellular metabolism, protein synthesis, and tissue repair. Enhanced oxygen and nutrient supply optimize aerobic metabolism, generate ATP efficiently, and minimize metabolic waste accumulation. These metabolic improvements reduce fatigue, enhance performance, and accelerate recovery, making CO₂ cryotherapy valuable for athletes, post-injury rehabilitation, and recovery optimization. By improving both oxygenation and nutrient transport, it creates ideal conditions for cellular repair and functional recovery.
Enhanced Lymphatic Drainage
CO₂ cryotherapy stimulates lymphatic vessel contractility, enhancing drainage through smooth muscle activation, hydrostatic pressure changes, and inflammatory mediator clearance. This facilitates removal of metabolic waste, excess fluid, and inflammatory molecules, supporting tissue homeostasis. Improved lymphatic function benefits immune response and local tissue health, reducing swelling, inflammation, and fluid accumulation. CO₂ therapy enhances lymphatic pumping, valve function, and vessel resilience, promoting unidirectional fluid flow and efficient clearance. Clinically, enhanced drainage aids range of motion, edema reduction, and recovery, especially after surgery, injury, or chronic inflammation. By optimizing lymphatic function, CO₂ cryotherapy accelerates tissue recovery and supports systemic health.
Reduction of Edema and Inflammation
CO₂ cryotherapy reduces edema and inflammation through multiple pathways: decreasing pro-inflammatory cytokines, enhancing anti-inflammatory mediator release, and improving tissue drainage. This leads to swelling reduction, pain relief, and improved function. It modulates the inflammatory cascade by suppressing NF-κB activation while increasing heat shock proteins and antioxidant activity, resolving acute inflammation and preventing chronic damage. Edema reduction is also achieved via enhanced lymphatic drainage, venous return, and reduced capillary permeability, minimizing fluid accumulation. These effects benefit conditions like lymphedema, chronic venous insufficiency, post-traumatic edema, and other inflammatory or fluid-retention disorders. By mitigating inflammation and promoting fluid clearance, CO₂ cryotherapy supports recovery, mobility, and tissue health.
Physiological Benefits of CO₂ Cryotherapy
The comprehensive effects of CO₂ cryotherapy on microcirculation translate into multiple physiological benefits that extend across various body systems and functional domains. These benefits result from the cascading effects of improved tissue perfusion, enhanced cellular metabolism, and optimized inflammatory responses that collectively support tissue health and functional performance. Understanding these diverse benefits provides context for the broad therapeutic applications of CO₂ cryotherapy while explaining the mechanisms underlying clinical observations across different patient populations and treatment conditions. The following sections explore the major physiological benefits and their underlying mechanisms.
Muscle Recovery and Performance
CO₂ cryotherapy enhances muscle recovery by improving microcirculation, increasing delivery of oxygen, nutrients, and growth factors essential for tissue repair and adaptation. Elevated blood flow facilitates removal of metabolic waste, including lactate, creatine kinase, and inflammatory mediators, reducing fatigue and accelerating recovery. Improved tissue oxygenation supports aerobic metabolism, ATP regeneration, and protein synthesis, crucial for muscle adaptation and hypertrophy. Studies show reduced markers of muscle damage and faster restoration of force capacity in athletes receiving CO₂ therapy. Performance benefits include reduced perceived exertion, enhanced power output, and improved endurance, resulting from improved circulation, reduced inflammation, and better metabolic efficiency. These effects make CO₂ cryotherapy particularly valuable for athletes needing rapid recovery between training sessions or competitions.
Pain Modulation
CO₂ cryotherapy provides analgesia via nociceptor desensitization, gate control mechanisms, and endorphin release, reducing pain perception and improving function. Cold exposure activates large sensory fibers that inhibit pain signal transmission through spinal gating. Enhanced microcirculation reduces tissue inflammation and ischemia, decreasing nociceptor sensitization. Improved blood flow facilitates removal of inflammatory mediators while delivering anti-inflammatory and analgesic compounds to affected tissues. Long-term benefits arise from improved tissue health, reduced chronic inflammation, and accelerated healing, addressing underlying causes of pain rather than merely masking symptoms. These mechanisms make CO₂ cryotherapy effective for acute pain management and chronic pain conditions, supporting functional recovery and overall comfort.
Joint Health and Mobility
CO₂ cryotherapy enhances microcirculation around joints, supporting synovial fluid production, cartilage nutrition, and removal of inflammatory products. Improved perfusion delivers nutrients for cartilage maintenance and facilitates clearance of catabolic enzymes and inflammatory mediators. The therapy reduces joint stiffness via enhanced tissue elasticity, reduced muscle guarding, and improved synovial fluid viscosity, promoting smooth movement and increased range of motion. Anti-inflammatory effects may slow degenerative changes by reducing cartilage-degrading enzyme activity and enhancing protective factor expression. These effects support joint health in aging populations and individuals at risk for osteoarthritis, improving functional mobility, flexibility, and overall joint resilience. CO₂ cryotherapy offers both preventive and therapeutic benefits for maintaining joint function.
Circulatory System Support
Regular CO₂ cryotherapy may benefit the circulatory system through improved endothelial function, vascular reactivity, and reduced chronic inflammation, supporting cardiovascular health. Controlled thermal stress promotes adaptations similar to exercise, including enhanced heart rate variability and blood pressure regulation. Improved microcirculation enhances tissue perfusion, benefiting individuals with peripheral vascular disease, diabetes-related circulation issues, or other perfusion impairments. These effects support wound healing, infection prevention, and tissue health. The stress adaptation induced by CO₂ therapy enhances cardiovascular resilience, improving the body’s ability to respond to physiological challenges. Such adaptations are valuable for older adults or those with cardiovascular risk factors, promoting overall vascular function, circulation, and systemic health.
Duration, Frequency, and Protocols
Optimal CO₂ cryotherapy protocols require careful consideration of treatment duration, frequency, and application parameters to maximize therapeutic benefit while ensuring safety and tolerability. The development of evidence-based protocols reflects advances in our understanding of dose-response relationships and individual variation in treatment response. The following sections provide guidance for developing effective CO₂ cryotherapy protocols based on current research and clinical experience, with emphasis on factors that influence treatment effectiveness and safety considerations for different patient populations and therapeutic goals.
Typical Session Duration and Temperature Ranges
Standard CO₂ cryotherapy sessions apply CO₂ at -78°C for 10–15 seconds per site, creating an optimal thermal gradient to trigger physiological responses while avoiding tissue damage. The brief exposure leverages the rapid onset of therapeutic effects, as benefits plateau after 10–15 seconds, with longer applications increasing risk without added gain. Typical treatment areas span 5–10 cm², with larger regions requiring overlapping applications to ensure full coverage. Precise temperature control in CO₂ systems allows consistent, reproducible therapy across anatomical sites and patient populations, balancing standardized protocols with flexibility for individual needs. This time-limited approach supports efficient multi-site treatments, maximizing safety and therapeutic efficacy in both clinical and athletic settings.
Recommended Frequency for Circulatory Benefits
For microcirculatory enhancement and general wellness, CO₂ cryotherapy is recommended 2–3 times per week, allowing adequate recovery while maintaining therapeutic momentum. Athletes or individuals with high recovery demands may use daily sessions during intensive training, with frequency tailored to individual response and recovery status. Monitoring subjective feedback, functional outcomes, and objective measures helps optimize treatment frequency. Long-term maintenance typically involves 1–2 sessions per week, preserving benefits while minimizing treatment burden. This approach supports sustained circulatory health and facilitates integration with other interventions, lifestyle routines, and recovery strategies. Adjusting frequency based on goals, individual responsiveness, and activity levels ensures safe, effective, and personalized circulatory support.
Factors Influencing Effectiveness
CO₂ cryotherapy effectiveness is influenced by individual factors including age, baseline cardiovascular health, fitness level, and circulatory conditions that affect vascular reactivity. Younger or healthier individuals generally respond more robustly, while older adults or those with vascular disorders may require protocol adjustments. Environmental conditions such as ambient temperature, humidity, and hydration also affect tolerability and outcomes, with optimal therapy performed under comfortable conditions with adequate hydration. Timing relative to exercise, meals, and daily activities impacts results: post-exercise application enhances recovery, while pre-exercise treatment may support performance through circulatory preparation. Understanding these factors enables clinicians and practitioners to personalize protocols for maximum therapeutic benefit and safety.
Evidence from Research
The scientific foundation supporting CO₂ cryotherapy applications in microcirculation enhancement continues to expand through controlled studies examining both acute responses and long-term adaptations. This research provides crucial evidence for understanding therapeutic mechanisms, optimizing protocols, and establishing appropriate clinical applications for diverse patient populations. The following sections review key research findings that support CO₂ cryotherapy applications while identifying areas where additional investigation is needed to fully establish evidence-based practice guidelines for different therapeutic contexts and patient populations.
Key Studies on CO₂ Cryotherapy and Microcirculation
Research using laser Doppler flowmetry shows that CO₂ cryotherapy significantly enhances microcirculatory blood flow, with peak increases above baseline occurring 10–15 minutes post-treatment and sustained elevations lasting 2–4 hours. Studies of endothelial function via flow-mediated vasodilation indicate improved vascular reactivity following repeated treatments, suggesting cumulative benefits mediated by increased nitric oxide availability and reduced oxidative stress. Investigations using near-infrared spectroscopy confirm that enhanced blood flow translates into improved tissue oxygenation, supporting metabolic activity and cellular recovery. These mechanistic findings provide a strong physiological basis for the observed benefits in muscle recovery, performance, and tissue repair, highlighting the efficacy of standard CO₂ cryotherapy protocols in improving microcirculatory and endothelial function across various clinical and athletic contexts.
Clinical Outcomes for Recovery and Pain Relief
Clinical trials in athletes show that CO₂ cryotherapy reduces exercise-induced muscle damage, lowers pain scores, and accelerates functional recovery following intense training or competition. In chronic pain populations, repeated treatments lead to significant improvements in pain intensity, functional capacity, and quality of life, indicating that enhanced circulation provides sustained benefits rather than temporary symptom relief. Biochemical studies reveal reduced pro-inflammatory cytokines and increased anti-inflammatory mediators, supporting the observed clinical improvements. Together, these findings demonstrate that CO₂ cryotherapy effectively promotes muscle recovery, pain relief, and anti-inflammatory effects, making it a valuable intervention in sports medicine, rehabilitation, and management of chronic inflammatory or pain conditions, while offering mechanistic evidence for its physiological and therapeutic impact.

Mögliche Risiken und Überlegungen
While CO₂ cryotherapy demonstrates excellent safety profiles when properly applied, understanding potential risks and contraindications ensures optimal patient safety and treatment outcomes. The extreme temperatures involved require careful attention to application techniques, exposure duration, and individual patient factors that might influence treatment safety or effectiveness. The following sections outline key safety considerations, contraindications, and risk management strategies that enable safe, effective CO₂ cryotherapy applications across diverse patient populations while maximizing therapeutic benefit and minimizing adverse event potential.
Physiological Stress and Overexposure
Excessive CO₂ cryotherapy exposure can cause tissue damage such as frostbite, nerve injury, or vascular compromise, highlighting the need to follow recommended 10–15 second application limits. Overexposure signs include persistent numbness, tissue discoloration, or unusual pain, which may require immediate medical evaluation. Individual sensitivity varies, so some patients may need shorter exposures or modified protocols to prevent adverse effects. Proper training in application techniques and careful monitoring of patient responses during initial sessions ensure safety and therapeutic effectiveness, allowing practitioners to identify patients who require special precautions or alternative approaches while maintaining optimal treatment outcomes.
Contraindications for Cardiovascular Conditions
CO₂ cryotherapy may not be suitable for patients with severe cardiovascular disease, uncontrolled hypertension, or recent cardiac events due to circulatory stress induced by cold exposure. Conditions like Raynaud’s phenomenon or cold-induced vasospasm can increase risk of excessive vasoconstriction, requiring careful evaluation or alternative therapies. Pregnancy, especially in the first trimester, represents a relative contraindication due to limited safety data and potential fetal risks from thermal stress. Medical clearance and conservative approaches are recommended for patients with cardiovascular risk factors or other conditions that could compromise treatment safety and efficacy, ensuring the therapy is applied only when appropriate.
Interactions with Medications or Supplements Affecting Circulation
Medications affecting circulation, blood clotting, or cardiovascular function can influence CO₂ cryotherapy responses, necessitating protocol adjustments or monitoring. Anticoagulants, vasodilators, and beta-blockers may alter expected effects, while supplements impacting circulation, inflammation, or thermoregulation may enhance or inhibit treatment responses. Although CO₂ cryotherapy is localized and non-systemic, patients taking multiple medications require careful evaluation to identify potential interactions or contraindications. Individualized treatment planning ensures safety and effectiveness, allowing practitioners to optimize therapeutic outcomes while minimizing risks associated with drugs or supplements that influence vascular or metabolic responses.
Practical Takeaways for Athletes and Physical Therapy
CO₂-Kryotherapie ist ein wertvolles Instrument for athletes and physical therapy, offering targeted microcirculatory benefits that complement traditional recovery and rehabilitation strategies. For athletes, applying CO₂ cryotherapy immediately after training or competition optimizes recovery, reduces tissue damage, and supports subsequent performance. Its brief 10–15 second application makes it practical in busy training environments. In physical therapy, CO₂ cryotherapy reduces pain and inflammation while promoting tissue healing through enhanced circulation, with precision that allows targeting specific regions without systemic interference. Integration with standard recovery protocols—proper nutrition, hydration, sleep, and progressive loading—ensures synergistic benefits rather than replacement of foundational practices. Long-term success requires consistent, evidence-based application, monitoring individual responses, and adjusting protocols as needed. With proven safety, measurable effectiveness, and practical convenience, CO₂ cryotherapy is positioned as a promising modality in sports medicine and rehabilitation, enhancing performance, supporting recovery, and offering flexible applications across diverse populations.